Authors / metadata
DOI: 10.36205/trocar2.2022001
Abstract
Introduction: Uro-gynecological issues affect women to the same extent worldwide. The requirements for treatment and the options available differ from region to region, from country to country.
Aim: The SIG Uro-Gynecology would like to give general recommendations to get a good diagnosis.
This is the basis of good treatment. SIG tries to consider the different possibilities of different continents, countries and regions.
Introduction
Pelvic floor defects are by definition a benign disease. This requires from us as doctors, in addition to considering the symptoms and defects, to also take the greatest care to produce the fewest possible side effects of our therapy. When treating malignant diseases, we often accept disturbances in the area of the nerves or vessels, since the treatment is about the survival of the patient. In the case of pelvic floor defects, a woman’s life can be very limited, but the condition is never life-threatening. For a long time, the reconstruction of the pelvic floor was mainly based on anatomical changes. This was reinforced by the focus on changing the POPQ before and after operations. In recent years, the focus has shifted more to “positive”, “functional” clinical changes and satisfaction scores have been introduced (1-6).
During the first decade of the third millennium the focus was still on increasing effectiveness and new materials and repair systems were sought after in order to be able to offer even longer-lasting processes. The risks were somewhat forgotten and new, sometimes severe complications led to bans and severe restrictions in the choice of therapy in many countries.
Therefore, a return to a good diagnosis is very important in order to be able to develop a therapy that is both tailored and as individual as possible for our patients. Because there is no one-fits-all solution, or it has been shown that these systems entail high risks, as they often generate over treatment (5).
Requirements for a good anamnesis
It is recommended to ask the patient for her complaints and let her speak an describe these in her own words. This is important because the extent of a pelvic floor defect does not necessarily correlate with the perceived symptoms. (Important Note: A patient without symptoms should not be treated surgically even if there are clear defects).
Since incontinence is often associated with pelvic floor defects, it is advisable to have the patient keep a voiding log for a week. It can also be very helpful in helping the patient understand the difference between SUI and Urgency. Especially with regard to symptoms after surgical therapy, it is important to document the symptoms in an understandable way so that they can be classified later with the patient.
It can be very helpful if you adopt a personal oral questioning scheme. However, some colleagues also prefer questionnaires regarding the symptoms or so-called quality of life questionnaires.
Important Symptoms:
- pelvic pressure
- urgency
- incontinence
- bleedings (erosion) (Pessary or mechanical due to prolapse) (uterus?)
- prolapse of the uterus or the vagina
- urinary retention
- Residual urine and chronic infections
- reduced Urinary Flow
Cases and reasons or side effects to be evaluated:
- Obstetric history
- Obesity?
- Previous surgery
- Medication
- Diabetes
- Nerve affections
Important is a basic analysis of the urine. Rapid tests (strip tests) have insufficient sensitivity, so in women with dysuria a urine culture with antibiogram should be performed. Strip test for screening for the detection of microhematuria Urine culture for urge incontinence to exclude bladder infection.
Residual urine determination, preferably sonographically, if necessary with a disposable catheter A residual urine of more than 50 ml immediately after micturition can be an indication of a bladder emptying disorder. If vaginal ultrasound is used for the measurement, 30 ml has been described as the upper limit of a normal residual volume, after single catheterization higher limits can be accepted. Note the renal conveying rate of 1– 14 ml/min, which can lead to incorrectly high values if not measured in time. Further clarification of the causes makes sense: e.g. obstruction of the urethra as a result of descensus or stricture due to trauma or inflammation, detrusor insufficiency of various origins such as neurological disease or posttraumatic. (surgery)
Role of Ultrasound
Ultrasound provides the examiner with a dynamic view of the pelvic floor. Perineal sonography can be performed with a curved array, but a vaginal probe is also very suitable for imaging the pelvic organs. It is particularly valuable to see the situation and relationship of the organs in normal position, but also in motion. The patient should be instructed to press in different strengths, but also to cough repeatedly. Thus, the bladder neck and bladder bottom can be displayed very well. Midline defect can be easily seen and the wall thickness of the anterior vaginal wall can be assessed very well.
The bladder neck and urethra are also very easy to illustrate and under stress the behavior of the organs can be represented. This in turn allows conclusions to be drawn about possible disturbing factors. For example, incorrectly positioned incontinence tapes that constrict the bladder neck under load can be seen on ultrasound without much practice.
Basic Parameters:
- Position and mobility of bladder neck Bladder neck descent – cut off value: 20 mm
- Bladder neck–symphysis distance (BSD): 20 – 30 mm
- Urethral inclination
- Retro vesical angle – normal value of 90–120°
- Urethral length: 30 – 45 mm
The so called “funneling” of the upper part of the urethra expresses a SUI, sometimes it is possible to detect a jet (Pic.: 1 )
It is also possible to observe the longitudinal movement of the pelvic floor. Especially dorsal, this indicates a high risk of recurrence for posterior defects. On the one hand, the stability of the pelvic floor muscles can be palpated well, especially the ability of the patient to actively control the muscles is very easy to check with palpation, but ultrasound can also visualize the concentric work of the muscles very well. This helps, above all, the patient to observe the activity of the muscles herself. This works very well with a normal vaginal probe. With ultrasound, an avulsion (rupture of the levator muscle) can be well excluded or confirmed (Pic.:2).
Pic 3-5 more give more examples or reasons for ultrasound evaluation
Defects and Symptoms
Apical Defect: Level 1
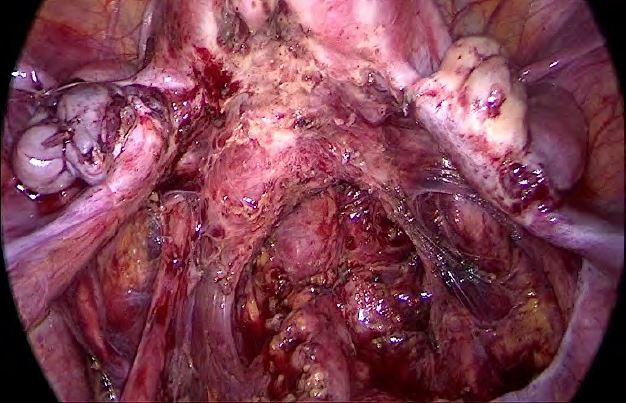
This describes the subsidence of the apical suspension of the pelvic floor, essentially the utero-sacral complex (Pic.: 6). This begins with the tissue that encircles the cervix and radiates laterally and dorsally to the deep pelvic wall. It is important to know that the fixation is low (S4-5) and not erroneously on S2. There you only find a duplicate in the peritoneum, which does not reach the sacrum!
The laxity of the USL complex often leads to the immersion of the uterus in the vagina and the resulting compression, it comes to the typical feeling of pressure and heaviness in the deep pelvis. Just over 50% of women report a chronic feeling of urgency of the bladder. This can be caused, among other things, by the stretching or compression of the deep nerve fibers. In about 80% of cases the urge improves or disappears after the prolapse is corrected (8).
Anterior Compartment: Level2
It is important to differentiate between lateral defect and mid line defect. Both usually occur in different decades and have distinguished origins. While the lateral defect is usually a delivery trauma with a strong elongation of the lateral parts of the pelvic fascia, the mid line defect develops over time. In pure form, both are easy to distinguish. The lateral defect is characterized by the fact that the rugae of the vagina are still completely or well preserved, but the vaginal wall passes between the labia. In the case of midline defects, the rugae are dissolved or hardly preserved. Midline defects (Pic.:7) are often associated with urinary retention, while in the case of lateral defects (Pic.:8), SUI dominates.
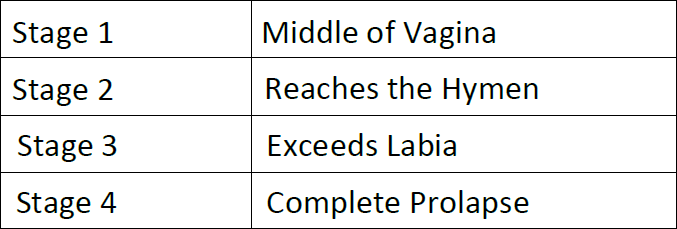
Posterior compartment: Level 2
The posterior vaginal wall can be overstretched by high weight and especially by delivery. The location of the defect results in different clinical symptoms. The upper third of the posterior vaginal wall forms a part of the pouch Douglas and is thus completely exposed to the pressures of the abdomen. The lower two-thirds form the dorsal end of the pelvic floor together with the rectum. If the patient developsarectocele (lower 2 thirds of the dorsal vagina), this can cause the rectal ampule to fill up excessively. On the one hand, this creates pressure in the pelvic floor and often leads to an outlet problem. In extreme cases, patients must digitally remove the stool. Strong pain by defecation can be an indication of an intussusception. This means an internal invagination of the rectum. This cannot be remedied by conventional gynecological techniques. Enterocele (upper third of the posterior vaginal wall) occur predominantly after hysterectomies or in the context Occasionally, due to a lack of good prior diagnosis, they occur after vaginal rectocele correction and then lead to pinching symptoms with pain. In the literature is used to classify the prolapse of POPQ. The nomenclature can be found online and in most text books. However, the system also knows the simpler graduation stage 1 to 4, which ultimately corresponds to the older Baden-Walker classification.
In the daily routine, therefore, graduation according to this simple system is often used. For example: Level 2 anterior midline Stage 2
Conclusion
Worldwide, there are very different ways to correct pelvic floor defects. However, the diagnosis and evaluation of complaints can be structured very uniformly and is decisive for the success of treatment. Anamnesis and gynecological examination are possible under simple conditions. Ultrasound examination by the gynecologist is not common in every country and perhaps the technical equipment is not available. However, this technique is very helpful to evaluate pelvic floor defects and if possible, urogynecologists should familiarize with the technique. The demand and expectations concerning treatment is also very heterogeneous and certainly differs culturally or in terms of standard of living, so no uniform recommendation can be given in this regard. The article tries to highlight the basis as well as the options in diagnostics and to underline the importance of good examination.
References
Pic.: 1 Funneling in case of SUI
Pic.2: Vaginal probe: dynamic examination of the levator muscles to exclude an avulsion and good representation of the pelvic floor muscles.
Pic.: 3 Twisted tape horizontal
Pic.4: Tape lying too high with a pointed retraction of the bladder.
Pic. 5: Midline Zystocele
Pic.6: In this picture (endometriosis surgery), the deep insertion of the USL is clearly understood. No currently existing technology can reconstruct this structure 1:1!
Pic 7: Midline defect
Pic.8: lateral defect