Authors / metadata
DOI: 10.36205/trocar5.2024011
Abstract
In 1996, we described Fertiloscopy as a minimally invasive diagnostic and therapeutic technique to evaluate and treat, in certain circumstances, female infertility. This technique combines hydrolaparoscopy, tubal patency test, salpingoscopy, sometimes microsalpingoscopy, and hysteroscopy to provide a thorough assessment of the female reproductive organs with minimal invasiveness.
Fertiloscopy offers several advantages, including enhanced visualization of pelvic structures, the ability to perform some therapeutic interventions during the same procedure, reduced recovery time, and the potential for outpatient treatment under local anesthesia. or general sedation. While laparoscopy remains the gold standard in certain clinical situations fertiloscopy presents a viable option for many patients, particularly those with no obvious pathology.
Introduction
Infertility affects millions of couples worldwide, often leading them to seek medical assistance to conceive. Infertility workups traditionally involve a range of diagnostic procedures, with laparoscopy long being considered the gold standard for evaluating and managing pelvic conditions.
However, the advent of fertiloscopy has introduced a minimally invasive, transvaginal approach that offers both diagnostic and therapeutic benefits. Despite its advantages, fertiloscopy remains underutilized, often overshadowed by other techniques. This article explores the evolution, indications, techniques, outcomes, and the current status of fertiloscopy in the management of infertility.
Historical Background
The roots of fertiloscopy can be traced back to the development of culdoscopy in 1948 by Decker and Cherry, which involved visualizing pelvic organs through the posterior vaginal fornix. While innovative, culdoscopy was eventually supplanted by laparoscopy due to the need to use the genu pectoral position for the patient at culdoscopy and the reporting of some cases of pelvic infection and the limited view of the pelvic structures (1,2). However, the idea of using a transvaginal route for pelvic exploration resurfaced in the late 20th century with the development of Transvaginal Hydrolaparoscopy (THL) by Gordts and colleagues in the 1990s. THL involved using saline to create a working space within the peritoneal cavity, providing enhanced visualization with minimal invasiveness (3). Building on these concepts, we have introduced the concept of fertiloscopy in 1996 as a combination of hydrolaparoscopy, salpingoscopy, microsalpingoscopy, and hysteroscopy, offering a thorough evaluation of the pelvic structures with reduced invasiveness and specific advantages such as the evaluation of the tubal mucosa by salpingoscopy compared to traditional laparoscopy.
Indications for Fertiloscopy
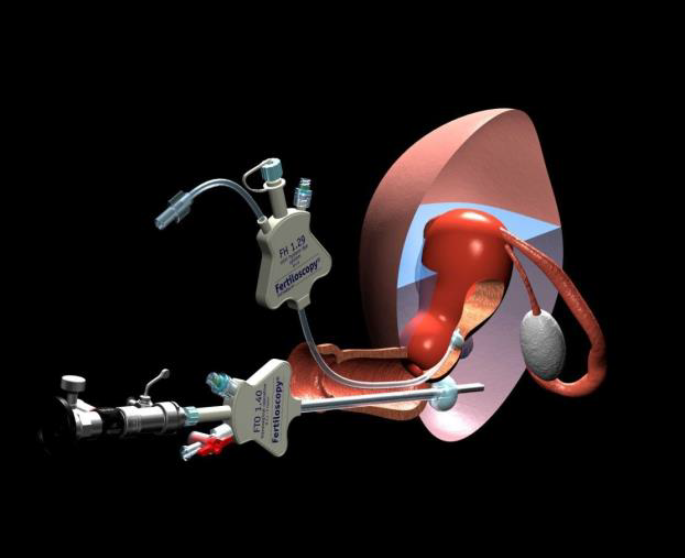
Fertiloscopy is particularly suited for patients with unexplained infertility where no obvious pelvic pathology is detected through non-invasive methods such as ultrasound or hysterosalpingography. It is probably the best tool for evaluating the patency and functionality of the fallopian tubes, as well as for detecting subtle forms of endometriosis, subtle abnormalities or adhesions that might not be visible through other imaging techniques. By providing both a diagnostic assessment and the potential for some therapeutic intervention at the same time, fertiloscopy is an effective option for patients who prefer to avoid the invasiveness of laparoscopy. Technique and Equipment (Fig.1,2).
We have described the technique in several publications (5,13) The principles are the following: Fertiloscopy is performed under local anesthesia or light general anesthesia similar to the one used for egg collection during IVF and is typically an outpatient or office procedure. The procedure begins with a diagnostic hysteroscopy to assess the uterine cavity for any abnormalities (6). Following this, a Veress needle is inserted in the pouch of Douglas and 150, 2OO cc ringers’ lactate are instilled thus creating a working space; then an hysteroscope of 2,9 mm in diameter with a 30° final lens is inserted through the posterior vaginal fornix (Fig.2) to access the peritoneal cavity, a method reminiscent of the original culdoscopy but enhanced by modern endoscopic technology. We designed a special disposable trocar to access the pouch of Douglas that we called the Fertiloscope® (Fertility Focus, UK). Fitted with a balloon at its extremity to prevent the risk to slip out of the peritoneal cavity during the procedure. Also, a 5 French operative channel allows to introduce some operative instruments such as scissors, biopsy forceps or bipolar electrode.
Unfortunately, this equipment is currently not available. Therefore, the technical alternative is represented by the use of a spring-loaded needle and a special trans vaginal reusable trocar (Karl Storz SE & Co KG Tuttlingen, Germany) which is the equivalent minus the balloon but the technique is very similar.
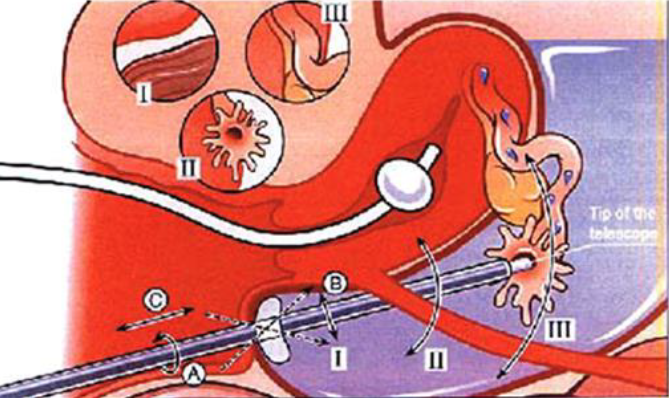
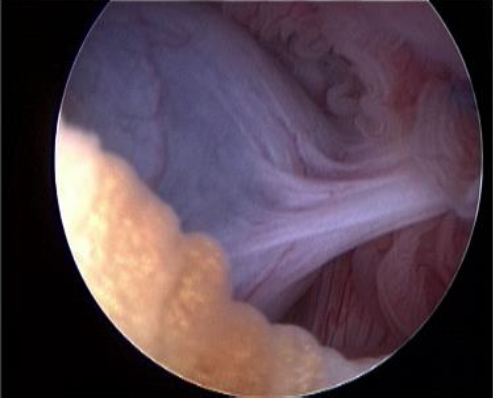
A key component of fertiloscopy is the integration of hydrolaparoscopy with a tubal patency test using methylene blue and salpingoscopy. Salpingoscopy involves the insertion of the same optic into the fallopian tubes to assess the tubal mucosa. One of the main technical advantages is the ability to perform salpingoscopy to evaluate the quality of tubal mucosa (Fig: 4,5,6,). Compared to laparoscopy where two endoscopes, two cold light supplies and two irrigation systems are needed, the same endoscope is used in fertiloscopy and in more than 95% of cases it is possible to enter at least in one tube (6) (Fig: 5,6,7).
This is further enhanced by microsalpingoscopy, described by Marana that allows for a more detailed evaluation of the quality of the mucosa by evaluating the proportion or tubal cell dye stained by the blue (4). The more the cells are dye stained, the more damaged the tubal mucosa is. We have to underline the fact that this microsalpingoscopy technique necessitates the use of the Hamou 2 hysteroscope (Karl Storz SE & Co KG Tuttlingen Germany). These types of scopes have a unique capacity to provide a magnification up to 100 allowing an in “vivo histology” of the tubal cells. Use of the saline solution during the procedure creates a working space that enhances the visualization of the pelvic organs, including the fallopian tubes, ovaries, and surrounding peritoneum in a physiological manner i.e. without the need to use any probe. Therefore, we see tubes and ovaries in their normal environment, even ovulation has been documented several times during fertiloscopy or THL (3).
After the procedure, the instruments are carefully removed, and the small vaginal incision closes naturally, reducing the risk of postoperative complications and facilitating a quick recovery (7).
If a pathology necessitates a further operative laparoscopy, it can be done immediately if the patient gave her consent or in a second time giving the time to explain the situation to the patients and giving time for her to decide which therapeutic options, she prefer usually a choice between tubal surgery and IVF. It is this latter approach that we favor.
Contra-indications
It is necessary to perform a vaginal examination prior to the procedure to detect any pathology of the pouch of Douglas and especially deep endometriosis of the cul de sac which would not allow to enter safely in the peritoneal cavity. Another contra indication is the presence of acute salpingitis. However, when the risk to encounter adhesions is high for example in patients having had peritonitis, it is always possible to perform a fertiloscopy since there is almost all the time a small space in the pouch of Douglas free of adhesions, and thus it is possible to evaluate if laparoscopy is worth to be performed or if IVF has to be directly proposed.
Complications
Fertiloscopy is generally considered a safe procedure, but like any surgical technique, it is not without risks. The primary complication associated with fertiloscopy is rectal injury during the introduction of the trocar. This complication occurs in approximately 0.6% to 1% of cases, particularly in the initial phase of a surgeon’s learning curve. As Gordts and Watrelot have noted, the risk of rectal injury decreases significantly after the first 20 to 30 procedures (9).
When a rectal injury occurs, the procedure should be halted and the patient should be placed on a 5-day course of antibiotics. Given that the injury is typically small, around 5 mm, and under the peritoneum thus without risk of contaminating the peritoneal cavity, no further surgical intervention is necessary.
Operative Fertiloscopy
Ovarian Drilling
One of the therapeutic procedures performed during fertiloscopy is ovarian drilling, particularly in patients with clomiphene-resistant polycystic ovary syndrome (PCOS). Ovarian drilling involves making small punctures in the ovarian surface, which can help restore normal ovulation in women with PCOS who have not responded to medical treatment.
During fertiloscopy, ovarian drilling can be performed under direct visualization with minimal trauma to the ovaries. (7,8,13). This approach has been shown to be effective in inducing ovulation and improving fertility outcomes in women with PCOS. The minimally invasive nature of fertiloscopy makes it an ideal platform for such procedures, combining the benefits of diagnostic assessment with the ability to address the underlying causes of infertility in a single session.
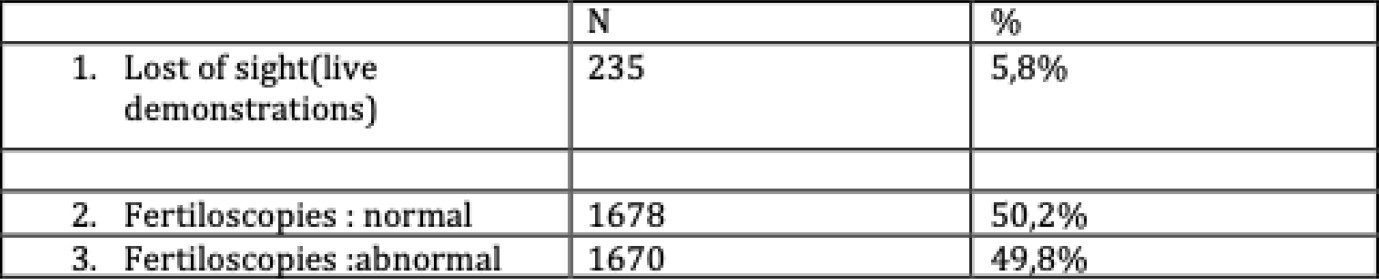
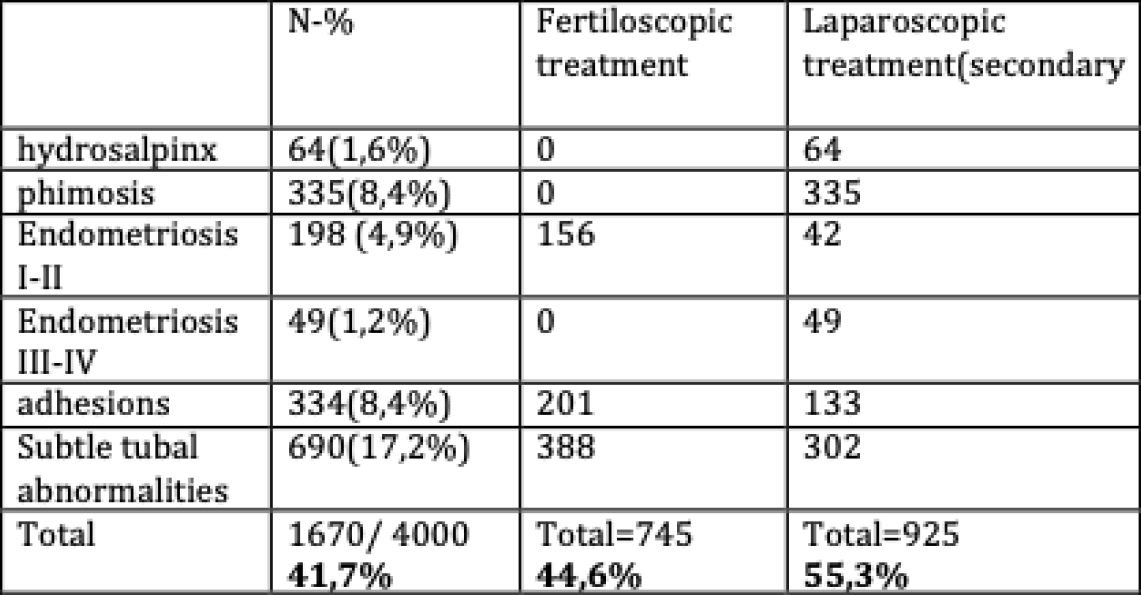
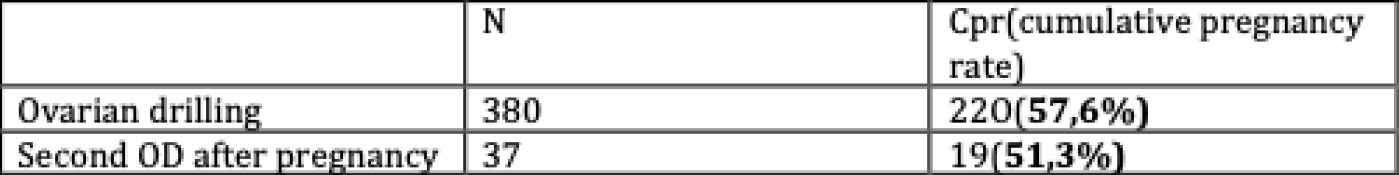
Personal results (Tab: 1,2)
Between 1996 and 2016, a series of 4,000 fertiloscopies have been performed by our team, providing quite extensive clinical experience and data on the efficacy and safety of this technique. This large-scale study allowed for the evaluation of fertiloscopy in various indications related to female infertility. Results are summarized (tab 1,2). It includes data on the number of cases diagnosed with pelvic adhesions, minimal endometriosis, and tubal abnormalities as well as the number of therapeutic procedures performed, such as adhesiolysis, treatment of minimal endometriosis, and ovarian drilling. The associated percentages illustrate the prevalence of the pathologies encountered and the success rate of the interventions carried out during these fertiloscopies. This table highlights the broad application of fertiloscopy in the management of female infertility and the effectiveness of this technique as a diagnostic and sometimes therapeutic tool.
In our series, 50,8% of fertiloscopies were normal leading the patients to be referred to ART.
In the other cases (49,2%) we were able to treat the abnormalities by means of fertiloscopy (adhesiolysis, coagulation of minimal endometriotic ovarian lesions, ablation of paratubal cyst – 44,6% of cases N=745). In the remaining cases (55,3% -N=925), operative laparoscopy was necessary for either hydrosalpinx or mild or severe endometriosis (Tab: 1).
Discussion: Advantages and Disadvantagesof fertiloscopy The Role of Fertiloscopy inInfertility Workups
Fertiloscopy occupies a prominent position in the spectrum of infertility diagnostics and treatment. It offers a minimally invasive alternative to laparoscopy, particularly for patients without obvious pelvic pathology.
Advantages of Fertiloscopy
1.Minimally Invasive Approach: Fertiloscopyis less invasive than laparoscopy, as it avoidsabdominal incisions and can be performedunder local anesthesia. This reduction insurgical trauma leads to faster recoverytimes, less postoperative pain, and a reduced risk of complications such as infections and adhesions (8, 9).
2.Enhanced Visualization: The combinationof hydrolaparoscopy with salpingoscopy andmicrosalpingoscopy in fertiloscopy enhancesthe visualization of the pelvic organs in theirnatural position. This allows for the detectionof subtle pathologies like peritonealadhesions, minimal endometriosis, and tubalanomalies that might be missed with othertechniques (10,11). Moreover, salpingoscopyis much easier to perform by fertiloscopythan by laparoscopy
3.Simultaneous Diagnostic and TherapeuticCapability: Fertiloscopy allows for both thediagnosis and immediate treatment ofidentified (but limited) pathologies, such asadhesiolysis for minor adhesions, treatmentof minimal endometriosis, correction ofminor tubal anomalies, and ovarian drillingfor clomiphene-resistant PCOS. This reducesthe need for additional operative laparoscopy.
4.Outpatient Procedure with QuickRecovery: As an outpatient procedure,fertiloscopy typically requires only a shortrecovery period, allowing patients to returnto normal activities much sooner comparedto those who undergo laparoscopy (13,14).
5.Cost-Effective: Due to its minimallyinvasive nature and the possibility of beingperformed under local anesthesia,fertiloscopy can be more cost-effective thanlaparoscopy, reducing the overall healthcarecosts associated with infertility treatment(17).
Disadvantages of Fertiloscopy
1.Technical Challenges: Fertiloscopy requiresspecialized training and experience,particularly due to its unique combination oftechniques and the transvaginal approach.Surgeons need to be adept at managing theconfined working space and using miniature instruments effectively (18).
2.Limited Visualization Compared toLaparoscopy: While fertiloscopy providesexcellent visualization of the pelvic organs, itdoes not offer the same comprehensive viewof the entire abdominal cavity aslaparoscopy. This limitation means thatfertiloscopy may not be suitable for patientswho rare suspect of pathology or withabnormal hysterosalpingography wherelaparoscopy will be needed (19)
3.Specific Complications: Although rare,complications such as bowel or bladderinjury and pelvic infections can occur due tothe transvaginal access route. Proper patientselection and surgeon expertise are crucial tominimizing these risks (9).
4.Limited Availability: Currently,fertiloscopy is not as widely available aslaparoscopy, particularly outside of Europe.This limited access can restrict its use tospecialized centers, making it less accessibleto a broader patient population.
Comparison with Laparoscopy
Laparoscopy has been the “gold standard” of infertility diagnosis and treatment for decades, providing a detailed exploration of the pelvic and abdominal cavities. It allows for the direct assessment and treatment of conditions such as endometriosis, pelvic adhesions, and tubal blockages, which are major contributors to infertility.
However, the emergence of fertiloscopy has introduced a new option for patients, particularly those who might benefit from a less invasive approach. A pivotal development in comparing these two techniques was the publication of the first prospective, double-blind, randomized study that directly compared fertiloscopy and laparoscopy in the management of infertility (12). This study was groundbreaking as it provided the first rigorous scientific comparison of two surgical techniques for infertility, challenging the long-held supremacy of laparoscopy.
Is Laparoscopy Still the Gold Standard?
The above study found that fertiloscopy offered comparable diagnostic accuracy to laparoscopy in identifying pelvic pathologies such as endometriosis and adhesions, which are critical in the evaluation of infertility (12). Furthermore, fertiloscopy presented several benefits, including a minimally invasive approach, reduced recovery time, and the ability to perform the procedure under local anesthesia—qualities that are particularly beneficial for patients who are reluctant to undergo more invasive procedures or have contraindications to general anesthesia.
Despite these advantages, laparoscopy retains several strengths that continue to justify its status as the gold standard in certain clinical situations. Laparoscopy provides a more comprehensive view of the abdominal cavity, making it suitable for patients with complex or extensive pathology such as endometriosis that may not be fully assessed through fertiloscopy. Moreover, laparoscopy’s established role in the surgical management of infertility, including its ability to perform more extensive surgical interventions, remains unparalleled by fertiloscopy in certain cases.
Discussion of the study and Its Implications
The prospective double-blind study underscored the importance of individualized patient care in infertility treatment. It highlighted that while fertiloscopy and laparoscopy each have their unique strengths, the choice between the two should be guided by the specific clinical situation and patient preferences. For instance, fertiloscopy might be preferable for patients with no obvious pathology, whereas laparoscopy would be more appropriate for those requiring a thorough abdominal exploration or when a surgical intervention is anticipated.
The findings suggest that fertiloscopy could serve as an initial diagnostic tool, reserving laparoscopy for cases where more extensive surgical intervention is needed or when the results obtained by fertiloscopy are inconclusive. This approach could optimize patient outcomes by reducing unnecessary surgical exposure while ensuring comprehensive care for more complex cases.
Why Fertiloscopy Might Become MoreWidespread
Several factors support the notion that fertiloscopy could become a more widely used technique in the diagnosis and treatment of infertility:
1.Advancements in Minimally InvasiveTechniques: As surgical techniques continueto evolve towards less invasive options, thereis an increasing preference for proceduresthat reduce patient recovery time, minimizesurgical risks, and that are cost-effective.Fertiloscopy fits well within this trend,offering a balanced approach betweeneffective diagnosis and treatment withminimal invasiveness.
2.Increasing Demand for OutpatientProcedures: Healthcare systems and patientsalike are leaning towards outpatientinterventions that allow for faster recoveryand reduced hospital stays. Fertiloscopy’sability to be performed on an outpatient basisaligns with this growing demand, potentiallymaking it a preferred option for patients andhealthcare providers
3.Expanded Access to Training: As morepractitioners become trained in fertiloscopyand its benefits become more widelyrecognized, it is likely that the technique willbecome more accessible. This increasedavailability could help in establishingfertiloscopy as a standard procedure in moremedical centers.
4.Supportive Clinical Evidence: Studies likethe prospective double-blind comparisonbetween fertiloscopy and laparoscopyprovide robust evidence supportingfertiloscopy’s efficacy. As more studiescorroborate these findings, the technique’sacceptance and adoption are likely to grow(12).
5.Patient Preferences: Patients increasinglyprefer less invasive procedures with quickerrecovery times and fewer postoperativecomplications. Fertiloscopy, with its minimalinvasiveness and effectiveness, is well-positioned to meet these patient preferences,driving its adoption in clinical practice
Conclusion
Fertiloscopy is positioned as a key tool in the diagnosis and treatment of infertility, particularly for patients for whom a less invasive approach is desirable. Compared to laparoscopy, fertiloscopy offers several advantages, including reduced invasiveness, quicker recovery, and the ability to be performed under local anesthesia. However, its limitations, such as restricted visualization and limited availability, mean that it is not suitable for all patients. The decision between fertiloscopy and laparoscopy should be tailored to the individual patient’s clinical needs, ensuring that each patient receives the most appropriate, effective, and least invasive care possible.
The first prospective, double-blind study comparing fertiloscopy and laparoscopy has provided crucial insights into the respective roles of these techniques, suggesting that the two techniques should be viewed not as competitors, but as complementary tools in the reproductive surgeon’s arsenal. As clinical evidence and practitioner experience with fertiloscopy continue to grow, it is likely that this technique will become more widely adopted, offering an effective and patient-friendly option in the management of infertility.
However, despite its early promise and popularity in the 2000s, fertiloscopy has not experienced the widespread adoption that was initially anticipated. In recent years, it has become somewhat overlooked, with reproductive specialists increasingly favoring direct IVF treatments when infertility presents without an obvious cause. It is unfortunate that a more thorough assessment, particularly through vaginal endoscopy, is not pursued more often before resorting to IVF. Fertiloscopy offers a minimally invasive option that can provide valuable diagnostic insights and therapeutic interventions, which might improve the chances of natural conception before moving to more invasive and costly fertility treatments like IVF.
References
Fig.1: principle of Fertiloscopy
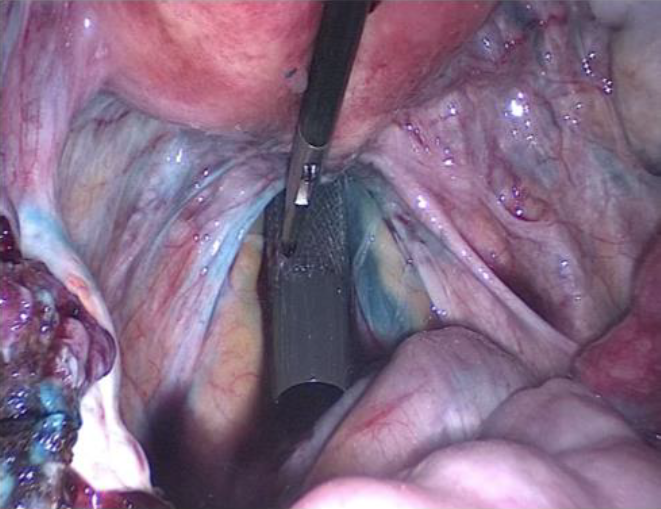
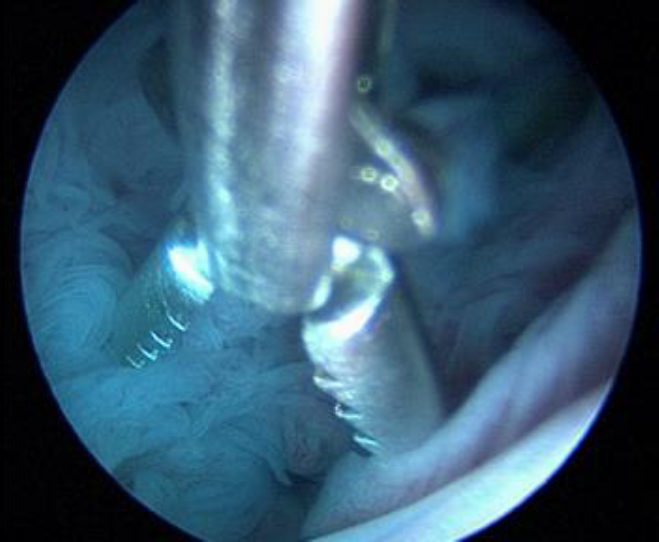
Fig.2: View by laparoscopy of the position on the transvaginal insertion of the optic in the pouch of Douglas
Fig 3: Priciple of fertiloscopy
Fig.4: fimbrial para tubal cyst
Fig.5: salpingoscopy: ampulalary view
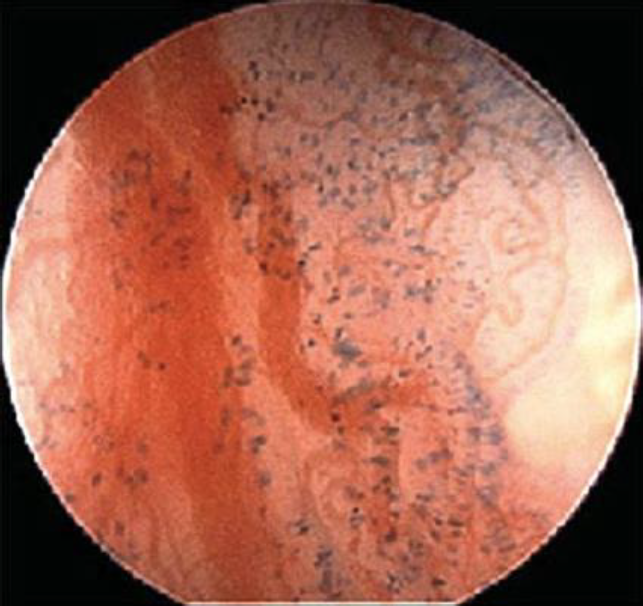
Fig.6: tubal cells, dye stained (m-blue)
Fig.:7 French instrument biopsy/ adhesiolysis
Table 1: results of 4000 fertiloscopies (French Académie of Surgery March 2016)
Table 2: results of ovarian drilling.