Authors / metadata
DOI: 10.36205/trocar6.2025002
Abstract
A definitive cervical cerclage, particularly a transabdominal cerclage (TAC), is a surgical intervention aimed at preventing late miscarriages and preterm labor in women with cervical insufficiency. This condition, often associated with recurrent late miscarriages or preterm births, can be challenging to manage, especially when conventional treatments such as progesterone or McDonald cerclage fail. While traditional guidelines typically recommend TAC only after multiple failed pregnancies despite cervical intervention, recent developments suggest that it may be beneficial in women with fewer previous miscarriages, particularly when a minimally invasive, effective, and reliable technique is available. This study reviews the outcomes of 70 patients who underwent laparoscopic TAC between 2018 and 2023, emphasizing a simplified technique that reduces operative time and minimizes complications. TAC before pregnancy was found to significantly improve pregnancy outcomes, with a high success rate and low complication rate, including in cases of concurrent endometrial conditions such as chronic endometritis.
The study also highlights the benefits of early intervention and the potential for expanding the indications for TAC, especially for women with one or two prior miscarriages. Our results suggest that, with careful patient selection and informed decision-making, TAC can be a valuable tool in preventing recurrent late miscarriages and improving pregnancy outcomes in women with cervical insufficiency.
Introduction
Cervical insufficiency affects up to 1% of the population and is a leading cause of late miscarriage between 14 and 23 weeks of gestation or premature labor. Diagnosis of cervical insufficiency is challenging as no specific diagnostic test exists, except in cases such as previous trachelectomy or extensive cone biopsy. Many examinations only prove to be inconclusive during pregnancy, making the patient’s obstetric history a crucial component of the diagnostic process. Treatment options during pregnancy are limited to progesterone or cerclage, both of which demonstrate suboptimal success rates. Classical vaginal cerclage procedures, such as McDonald or Shirodkar, are often proposed at the end of the first trimester, but their efficacy remains limited. An alternative approach, known as “definitive cerclage,” has been suggested either via a vaginal route (supracervical cerclage) or transabdominal route, the latter first described by Benson in 1965 (1). Trans Abdominal Cerclage (TAC) can be performed by laparotomy but is increasingly performed laparoscopically, sometimes with robotic assistance. In this article a simplified laparoscopic TAC technique is described. Traditionally, indications for definitive cerclage have been rare, typically offered only after two late miscarriages, plus a third miscarriage following a McDonald or Shirodkar cerclage performed at 12 weeks’ gestation. However, by proposing a simpler, faster, reliable, and minimally invasive technique, it is believed that indications for TAC could be expanded to include patients who have experienced one or two late miscarriages or a McDonald cerclage failure.
Materials and Methods
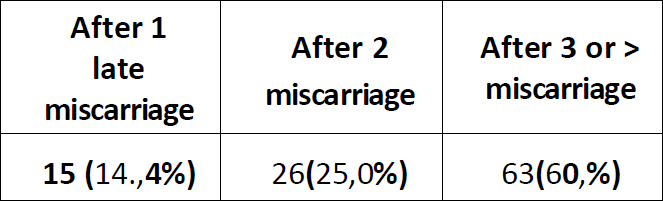
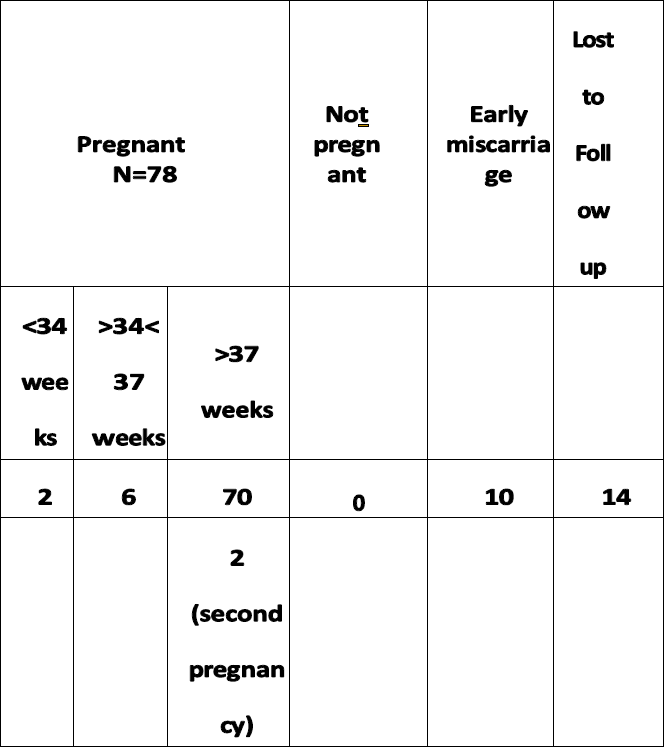
Patients: Between 2018 and 2023, 104 patients underwent laparoscopic cerclage using our simplified technique. Initially. The procedure has been limited to patients who had experienced three late miscarriages, but the indication was expanded to patients with one or two miscarriages after recognizing the profound emotional toll these events had on patients (Table 1).
All patients were informed that cesarean delivery would be required after the procedure. Patients were given a period for reflection, and written informed consent was obtained. While the aim was to perform the laparoscopic cerclage before a new pregnancy, some procedures were performed during the first trimester.
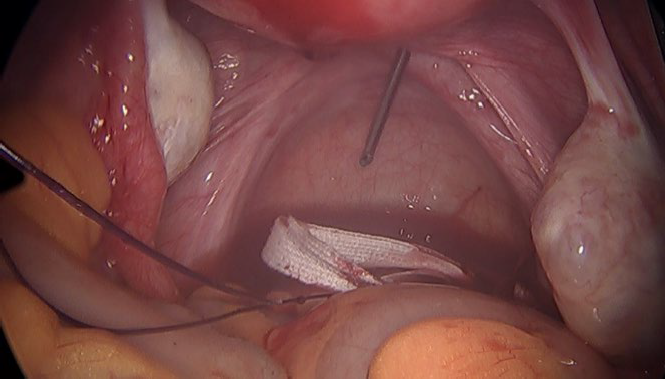
Surgical Method: The operation stated with a diagnostic hysteroscopy to identify and treat any intra cavitary abnormalities, and an endometrial biopsy was performed to assess for Impaired Inflammatory State of the Endometrium (IISE). A Hegar dilator No. eight was introduced into the cervix to facilitate spontaneous uterine evacuation or aspiration in cases of early miscarriage up to 13 weeks’ gestation. The dilator was also useful for uterine manipulation. Laparoscopy was initiated with a ten mm umbilical optical trocar, along with three five mm trocars for instrumentation in the lower abdomen. Following inspection, the peritoneum of the anterior cul-de-sac was opened, and a limited bladder dissection was performed to access the isthmus (Fig 1 to 5.)
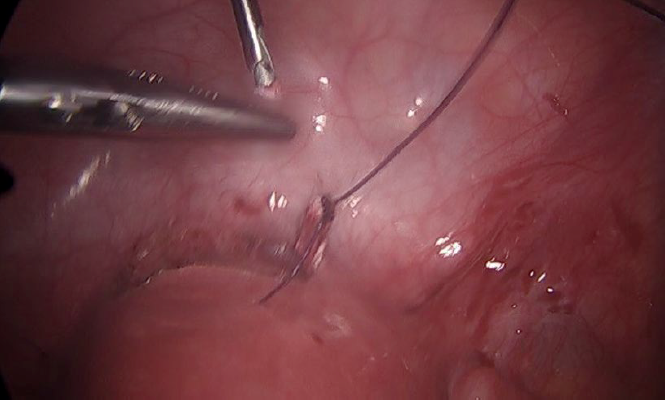
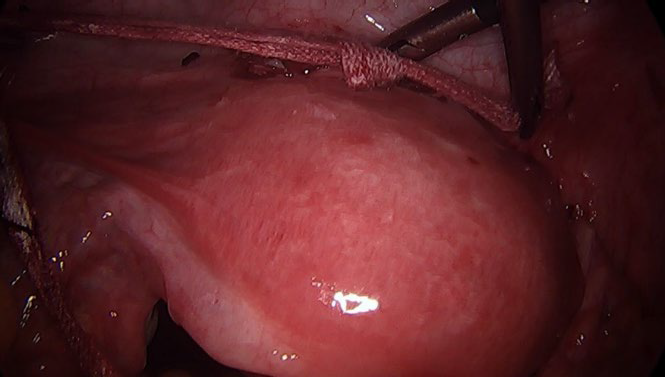
A Mersilene® mesh was introduced into the abdomen via a lateral port and left in the pouch of Douglas. An EndoClose® needle (Medtronic, Dublin, Ireland), a needle with a mobile eye for insertion of the tread, was used. The needle was introduced percutaneously just above the uterine isthmus and inserted in the cervix on the inside the uterine vessels. The needle then passed into the pouch of Douglas without requiring tunnel dissection, shortening the procedure. The needle was opened, and one end of the mesh was inserted. The process was repeated on the opposite side. Any minor bleeding that occurred typically resolved after knotting the mesh. The mesh was tied anteriorly, and the peritoneum was closed using Monocryl® 0 (Ethicon, New Jersey, USA), completing the procedure. The obstetricians were instructed not to remove the mesh during cesarean section, allowing for multiple pregnancies if desired.
Results
As many patients (n=59) were living outside of the region (Rhône, France) a web-based survey to assess mid- and long-term outcomes was conceived. 59 patients received the questionnaire. The outcomes of the other patients were already known(N-45). Of the 59 patients in the first group, 45 (76.3%) responded to the questionnaire, 14 patients were lost to follow-up. The average patient age was 28 years (range: 23–38 years). Before TAC, 15 patients had experienced one late miscarriage, 26 had two miscarriages, and 63 had three or more miscarriages. Additionally, 45 patients (63.3%) had previously undergone Shirodkar or McDonald cerclage in a prior pregnancy, with 11requiring emergency cerclage between 17–20 weeks. All of these patients experienced a preterm delivery, with only one newborn surviving (delivered at 23 weeks). In total, 101 TAC procedures have been performed prior to a pregnancy and three during pregnancy (eight to ten weeks’ gestation). Concurrent hysteroscopy was performed in 101 patients, with IISE detected in 18 cases (17.8%). These patients received a one-month course of antibiotics (minocycline) before attempting pregnancy. Patients were routinely advised to avoid getting pregnant for one-month post-surgery. Most patients were discharged on the same day or the day after surgery. The average laparoscopic time was 14 minutes (range: 10–23 minutes) in non- pregnant patients without associated pathology. In pregnant patients, the operating time was 30, 44, and 29 minutes, corresponding to ten (n:2) and 8 weeks of pregnancy, respectively. Out the 104 patients, three experienced minor complications, including scar defects that required nursing care. During laparoscopic TAC, the following associated conditions have been treated: endometriosis (n=7; five stage II, and two stage I according to the AFS classification), myoma removal (n=3), and extensive adhesiolysis (n=7). Aside from the extended operating times, these conditions did not result in any significant complications.
Pregnancy Outcomes:
Among the 45 patients who responded to the survey, 36 became pregnant following TAC (80%). Among the 49 other patients 39 became pregnant (79,5%). In all, three patients were pregnant at the time of the operation and 75 after cerclage (74,2%). Ten patients experienced first-trimester miscarriages (10/101= 9,9%): seven spontaneous expulsions and three requiring aspirations. The cerclage did not present an obstacle in any of these cases. No ectopic pregnancies occurred. Three patients opted to postpone a pregnancy for personal reasons. One patient delivered at 23 weeks due to chorioamnionitis and required cesarean delivery. Fortunately, the newborn survived. Another patient who underwent TAC at ten weeks with a twin pregnancy developed spontaneous labor at 20 weeks due to a myoma near the isthmus. After an unsuccessful attempt to remove the cerclage, a cesarean section was performed. In a later stage a laparoscopic myomectomy was performed and the TAC repeated. This patient eventually delivered a healthy baby at 37 weeks. In other pregnancies, cesarean sections were performed at 34 weeks in 4 patients, 35 weeks in 2 patients, and at 37 weeks in 59 patients (90,7%). All of the newborns, 61(twin pregnancies n=2) appeared to be healthy. Two patients experienced a second successful pregnancy without complications; their cerclage remained functional, and both delivered at over 38 weeks via cesarean section (Table2).
Discussion
This study describes a simplified TAC technique. Although retrospective, our series is larger than previously published reports (2-4). In non-pregnant patients, the operative time was significantly shorter compared to published techniques, which average 35–65 minutes, surgery time being even longer with robotic assistance (5). Performing TAC before pregnancy is preferred, as it facilitates easier dissection and uterine manipulation, with clearer landmarks visible (6,7). This approach is consistent with previous studies (8) and results in shorter procedures compared to surgeries performed during pregnancy (14 minutes vs. 30 minutes on average). Additionally, pre-pregnancy TAC enables concurrent hysteroscopy, which detected IISE in 17.8% of the cases. Although one case of chorioamnionitis at 23 weeks was confirmed, identifying IISE preoperatively may reduce the risk of chorioamnionitis. Our simplified technique also ensures that the cervix is not completely sealed, allowing for uterine evacuation in cases of first-trimester miscarriage. Alternative approaches include supracervical cerclage via the vaginal route at the end of the first trimester (9,10). However, due to complications such as infection and bleeding, we favor the laparoscopic approach. Moreover, laparoscopic TAC is performed at a higher level than the vaginal techniques, which may explain its positive outcome even when the cervix is short or absent, as seen after trachelectomy. Several studies support the superiority of laparoscopic approaches over vaginal approaches (2). Some argue that laparoscopy may hinder future pregnancies, but our data show a 91.1% pregnancy rate, consistent with the published literature. Moreover, the delivery of 39 healthy babies (95.1%) out of 41 pregnancies supports the efficacy of our simplified approach (11). While laparotomy remains an option, laparoscopy provides equivalent results with less invasiveness and should be favored (8).
Conclusion
TAC is a valid option for preventing preterm labor and late miscarriages. Our simplified technique is fast, reliable, and minimally invasive. With proper patient counseling and shared decision-making, TAC may be considered after one or two late miscarriages. The necessity of cesarean delivery is a minor inconvenience compared to the benefits of the procedure.
References
Table 1: Indications
Figure 1: Opening of the anterior cul de sac and the percutaneous insertion of the EndoClose needle
Figure 2: EndoClose is passed just above the uterosacral ligament and will take the thread attached to the mesh
Figure 3: the mesh is passed laterally, the same procedure is performed on the right
Figure 4: the anterior knot is closed.
Figure 5: end result before cul de sac peritonialization
Tabel 2: Outcome after Trans Abdominal Cerclage (TAC) (n=104)