Authors / metadata
DOI: 10.36205/trocar6.2025004
Abstract
In this study the objective is to report a case of abscessed appendico-cutaneous fistula in a 52-year-old blind patient who presents a long-standing clinical picture, characterized by intense pain in the abdominal and inguinal region. Contrast-enhanced computed tomography of the abdomen reported a collection in the adipose tissue and muscle plane in the right iliac fossa and hypogastrium with a volume of 810 cm3, appendix in infra-cecal position with its tip projected inside the right inguinal canal in contact with the collection. The approach was initially percutaneous drainage to manage the abdominal wall abscess, then an exploratory laparoscopic approach, where the appendix was identified embedded in the abdominal wall towards the inguinal region, crossing it, with the tip located in the abscessed mass within the subcutaneous cellular tissue of the region. The patient was discharged on the eighth postoperative day due to a favorable evolution, returning to his activities after five weeks.
Study Objective: To present the clinical case, since it is a fairly rare pathology, in which the resolution was hybrid, between a conventional approach to drain the abscess and a laparoscopic approach for the resolution of the intra-abdominal appendicular part.
Introduction
A fistula is an extra-anatomical communication between two or more epithelialized body cavities or with the skin surface (1). They can be classified according to their anatomical location, a fistula can originate in all segments of the urinary tract, digestive tract, genital tract, peritoneum and skin (2). The most frequent appendicular fistulas are those internal to hollow viscera, in order of frequency appendico-vesical, appendicointestinal (ileum, cecum, duodenum, ascending colon and Meckel’s diverticulum) and appendico-uterine, while appendico – cutaneous fistulas are extremely rare (3,4). In the literature, the first reported appendico-cutaneous fistula was found by Volz in the autopsy in 1846 (5). Subsequently, the reported cases of appendico-cutaneous fistula are few as it is an infrequent entity (6). When an untreated inflamed appendix progresses to suppuration, the usual course is rupture with abscess formation. In rare cases, acute appendicitis is resolved by fixation of the appendix to an adjacent viscus or to the parietal peritoneum and from there to the skin, which allows drainage of pus into the viscus or to the exterior. Cutaneous fistula can develop after drainage of an appendix abscess or secondary to an appendectomy (7). It can also develop spontaneously as a complication of acutely perforating appendicitis (8). The infectious process in the abdominal wall is a clinical picture that frequently occurs in surgical departments, it is of an extreme severity and with possible terrible consequences such as septic shock and multisystem organ failure (9).
Case Report
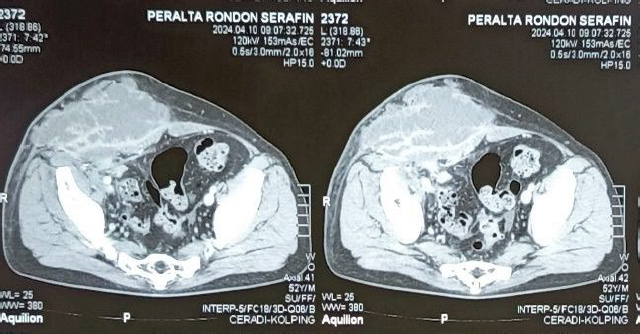
A 52-year-old blind man with a chronic clinical picture characterized by intense pain in the abdominal and inguinal region, for which he selfmedicated with analgesics and antiinflammatory drugs, as well as antibiotics (ATB). On physical examination: Abdomen: protruding erythematous mass of semi-hard consistency in the abdominal wall occupying the hypogastrium, iliac fossa, part of the flank and right inguinal region of approximately 15×10 cm with the presence of a crust with low-flow purulent fluctuation, decreased hydro-aerial sounds. Laboratory tests were performed: leukocytes: 17,000 x mm3, hematocrit: 37.7%, hemoglobin:12.4 g/dl. C-reactive protein: 131.2 mg/L and increased alkaline phosphatase 152 IU/L. Ultrasound reports a hypoechoic image with poorly defined irregular edges, extending upward to the right lumbar region, downward to the right inguinal and femoral region, presence of low intensity echoes compatible with collection. Computed axial tomography of the abdomen with contrast reports a collection in the adipose tissue and muscle plane in the right iliac fossa and hypogastrium with a volume of 810 cm3, appendix in infracecal position with tip projected inside the right inguinal canal in contact with the collection. (Fig. 1)
Interventions
Step 1
Conventional drainage of abscess time The patient was placed in a supine position and the surgery was performed under general anesthesia. Initially, percutaneous drainage was performed with several two cm incisions in the right iliac fossa and inguinal region on the same sides, with a preference for areas with a major slope, to first manage the drainage of the abscess of soft tissue within the abdominal wall. A purulent discharge and an evacuation of devitalized tissues in of approximately 800 cc was observed. The region with the abscess was washed with Dakin-Carrel solution. After digital examination, an area in possible contact with the retroperitoneum and internal surface of the iliac bone was identified. Laparoscopic appendectomy procedure Step 1 Introduction of trocars in the second stage, an exploratory laparoscopy was started, placing the patient in a supine position and in Trendelenburg position with a 15° rotation to the left, with the arms at the sides of the body. Pneumoperitoneum was achieved using the trans umbilical technique and laparoscopic trocars were placed using the American technique as follows: one ten mm trocar in the navel for the 30° degree fore oblique laparoscope, two ten mm trocar under direct vision in the left iliac fossa, three five mm trocar in the midline two finger-widths above the pubic spine.
Step 2 Inspection of the abdominal cavity
In the right iliac fossa and lateral wall of the right flank, the plastron is observed, with loops of small intestine and caecum firmly adherent to the wall of the region (Fig 2).
Step 3 Release of the plastron
A plastron is evident in the ileocecal region, formed by an intestinal loop. The cecum and terminal ileum are identified, attached to the abdominal wall with a fibrous process (Fig.3). The stump is then released using blunt and cutting maneuvers. A hole with purulent material is identified on the lateral wall of the inner face of the iliac bone, retroperitoneum at the level of the mid-axillary line, and a soft cecal appendix is also identified in the tract (Fig.4) and a sectioned appendicular base at the level of the cecal base.
Step 4 Enterorrhaphy of the appendicular stump
Enterorrhaphy in two planes: one plane with transfixion stitches with vicryl thread No. 3-0 and two planes with invaginating stitches with silk thread No. 3-0, revision of the appendicular base revealed no leak or hemorrhage, satisfactory hemostasis was obtained (Fig. 5)
Step 5 Fistula orifice
Curettage of a fistulous orifice of approximately two cm where the smoothed cecal appendix was located. A Penrose drain is left in the bloody space through the same path of the fistula leading to the superficial abdominal wall and exteriorized by an opening in the skin, placing a tubular drain in the rectovesical recess with external drainage towards the left iliac fossa.
Measurements and main results
The percutaneous drainage lasted for 45 min and the exploratory laparoscopy for 130 min. The hydro procedure lasted for 175 minutes and the estimated blood loss was 150 ml. The patient followed a progressive hydro liquid diet for 12 hours after the procedure. The patient had an uncomplicated intraoperative and postoperative course, was treated with broad spectrum antibiotics (metronidazole and imipenem) and was discharged on the eighth postoperative day with laminar drainage, followed up with controlled dressings for 21 days with a noticeable improvement of the infection. The culture and antibiogram examination reported purulent fluid and gram-negative cocci. He was able to return to his daily activities 25 days after surgery. At her 5-week follow-up, she reported resolution of his symptoms.
Discussion
Although appendico-vesical and appendicointestinal fistulas are rare, an appendicocutaneous fistula is even more uncommon and offers a diagnostic challenge as a cause of the fistula (4,5). According to Kjellman, the main mechanism of fistula formation is the spontaneous rupture of the inflamed appendix into the adjacent intestine or the skin and the persistence of the fistula is due to the presence of an appendicular stone or carcinoid tumor or tuberculosis (5). In our case, both causes were ruled out. Cutaneous openings have been reported in the lower right quadrant of the anterior abdominal wall and even in other locations such as the right gluteus (10). In this case, the fistulous tract was found from the abdominal cavity, through the lateral wall of the right iliac fossa, with an oblique tract externalized towards the anterolateral wall of the right iliac fossa with the presence of a subcutaneous abscess in it. In most of the reported cases, computed tomography (CT) has been used as the primary modality for definitive diagnosis. Abdominal CT helps not only to establish the diagnosis but also to assess the extent of involvement (7). In the present case, the CT reported that the appendix was located in the external inguinal orifice, however, during the surgery, it was shown that this was not the case. To determine the source of a fistula, the fistulogram is the ideal method. However, it was not possible to perform it in the present case (7). It is important to emphasize the fact that the cecal base was found sectioned, without the presence of abscess, fistula or greater involvement at this level, during the intraoperative period. This leads us to assume that there was a fistulous tract established from the abdominal cavity towards the subcutaneous cellular tissue of the abdominal wall of the right iliac fossa.
Conclusion
In the reviewed literature, in many cases the laparotomy approach is the first choice, allowing the resolution of the condition, with the necessary technical and therapeutic possibilities, according to the intraoperative findings. The minimally invasive surgical approach offers the advantages of the technique, where the necessary procedures can also be performed according to what is identified during the surgery, thanks to the vast current technical possibilities offered by laparoscopic surgery, and/or hybrid procedures in trained hands, as in the present case. Laparoscopic surgery is a good therapeutic option, due to its high magnification, less surgical trauma, the feasibility of performing more complex procedures (example: complex Ileo-transverse resections with mechanical anastomoses, etc.), less postoperative pain for the patient and shorter hospital-stay. The best parameter for the resolution of this disease is definitely early diagnosis and once the patient’s surgical situation has been established, no resources should be spared to achieve proper treatment according to the severity of the pathology found.
References
Figure 1: Contrast-enhanced computed tomography of the abdomen small intestine, terminal ileum and cecum firmly adherent to the lateral wall of the region.
Figure 2: Cecum and terminal ileum adhered to abdominal wall with fibrous process suggestive of plastron
Figure 3: Hole with purulent material exiting on lateral wall, also lysed cecal appendix in the tract
Fig. 4 Intact appendicular base sectioned in the caecum
Figure 5: Repair of appendicular base by enterorrhaphy in two planes