Authors / metadata
DOI: 10.36205/trocar5.2024019
Abstract
Ectopic pregnancy is the leading cause of death in the first trimester of pregnancy. Its incidence has increased due to sexually transmitted diseases, the use of intrauterine devices and assisted reproduction techniques. Laparoscopic surgery has proved to be less invasive and traumatic. In addition to using vasopressin to control bleeding, additional techniques such as a precise incision with a fine monopolar cut may be considered. It is useful to make the incision in the antimesenterial region of the affected tube, starting from the proximal end of the ectopic pregnancy, and to avoid suturing the tube in the process. Laparoscopic salpingostomy not only maintains tubal patency, but also favors a better pregnancy rate after the procedure, so it is crucial to carefully select patients and perform rigorous follow-up to optimize long-term reproductive results. The article analyzes laparoscopic salpingostomy as an effective option to manage ectopic pregnancy, preserve fertility and minimize risks.
Introduction
Implantation of trophoblastic tissue outside the uterine cavity is a potentially life-threatening obstetric condition that occurs in approximately 2% of cases. Of these, 90% are located in the ampullary region of the fallopian tube and less than 1% in the intramural region, where the major complication is rupture and hemorrhage Interstitial ectopic pregnancies are documented in 2-3% of cases, where the blastocyst implants at the proximal end of the fallopian tube, penetrating the surrounding myometrium. This condition is responsible for 10-15% of pregnancy-related maternal deaths in developed countries, as well as the leading cause of death during the first trimester of pregnancy, accounting for 4-6% of all pregnancy-related deaths. Over time, there has been an increase in the incidence of these cases, attributed to the increase in sexually transmitted diseases, the use of intrauterine devices and assisted reproduction techniques. This anomalous implantation is usually the result of direct or indirect damage to the fallopian tubes (1). The pathophysiological mechanism leading to ectopic pregnancy is still not completely clear. However, several potential factors have been identified, such as defective ciliary movement and abnormalities in the muscular contractions of the fallopian tubes, as well as a proinflammatory environment associated with a history of infections or smoking. One proposed mechanism is the decrease in adrenomedullin, a calcitonin-related peptide expressed in the apical region of the fallopian tubes. This peptide plays a crucial role in stimulating ciliary movement and tubal contractions, and its reduction could contribute to the formation of ectopic pregnancies. Another factor implicated is the increase in interleukin 6 and interleukin 8, as well as tumor necrosis factor, which are elevated both in serum and in the tubes of patients with ectopic pregnancies. These inflammatory mechanisms alter embryo transport, favoring the adherence of the blastocyst to the tubal epithelium.
Historically, the treatment of ectopic pregnancy was exclusively managed by open procedures that carried a significant risk of morbidity and a prolonged recovery. However, the development of laparoscopic surgery in recent decades has revolutionized the management of this condition, offering a minimally invasive approach that considerably reduces recovery time, postoperative pain and complications, while preserving fertility in young patients (2). Currently, laparoscopy is considered the standard surgical approach for the management of ectopic pregnancy, and can be performed using two main techniques: salpingectomy (involving complete removal of the affected fallopian tube) and salpingostomy (incision into the tube to remove only the affected tubal tissue, allowing preservation of the tube). Although both procedures offer similar results, salpingectomy could present a potential disadvantage due to the interruption of utero-ovarian circulation and possible impairment of ovarian function, given that the tubal and ovarian arteries are close in origin (3).
Laparoscopic salpingostomy, in particular, has gained ground as a better conservative treatment option for women who wish to preserve their fertility, because as mentioned above it involves removing only the trophoblastic tissue, followed by secondary healing without the need for suturing, which helps maintain the anatomical and functional integrity of the tube. Several studies have shown that the rate of future pregnancies is significantly higher in women who undergo salpingostomy compared to those who undergo salpingectomy, as the latter technique removes a critical part of the female reproductive system. In a retrospective cohort study conducted in Quebec, two groups of women were compared: one treated surgically for an ectopic pregnancy, and the second, with intrauterine pregnancies. Among patients undergoing salpingectomy, the risk of a second ectopic pregnancy was 14%, while for those treated with salpingostomy, the risk rose to 21.9%, regardless of age. In addition, the study revealed that 0.72% of patients treated with salpingectomy experienced a second intrauterine pregnancy, compared to 0.89% in the salpingostomy group (12). The main advantage of the above is the high surgical success rate, which reaches between 87% and 97%, even in hemodynamically unstable patients. This technique reduces operative time, which decreases the risk of thromboembolic events and bleeding, and contributes to fewer postoperative complications. In addition, it shortens the hospital stay, which reduces costs for both the patient and the institution. It also allows for faster recovery, less use of pain medications, and offers better cosmetic results (4).
Conservative management of ectopic pregnancy, however, is not without risks. Patients undergoing laparoscopic salpingostomy have a slightly higher risk of recurrent ectopic pregnancy, which requires careful postoperative follow-up to detect any early complications (5). Furthermore, it is important that patients be properly selected for this procedure, considering factors such as hemodynamic stability, desire for future fertility, and absence of severe tubal damage (4).
This article focuses on the use of laparoscopic salpingostomy as an effective and safe surgical strategy for the management of ectopic pregnancy, especially in young women who wish to preserve their fertility. Through the presentation of a clinical case and the review of existing literature, the benefits of this technique are discussed, as well as the clinical considerations necessary to optimize reproductive outcomes and minimize associated risks.
Case Report
The case of a 23-year-old patient with a history of obstetric G4C1A2E1 who came to the emergency department due to a 6-day history of colicky pain is presented. The intensity of the pain was rated at 9 out of 10 on the visual analogue scale, located in the right iliac fossa and radiated to the right hypochondrium, accompanied by scant transvaginal bleeding. Relevant medical history includes a laparoscopic appendectomy performed 6 years ago and the use of combined oral contraceptives as a family planning method. The patient had never had a cervical cytology and her last menstruation occurred 2 months before her admission.
On the same day, an ultrasound was performed which showed endometrial thickening (11.2 mm), and no signs of intrauterine pregnancy. Subsequently, during her hospital stay, a new transvaginal ultrasound was performed, which revealed a hypoechoic mass of 24 x 24 millimeters in the right adnexa, with abundant free fluid in the posterior cul-de-sac. A pregnancy test was requested, which was positive, with a gonadotropin quantification of 1110.5 mIU/mL. The pelvic examination showed a painful abdomen, with signs of peritoneal irritation and transvaginal bleeding, as well as pain on cervical motion.
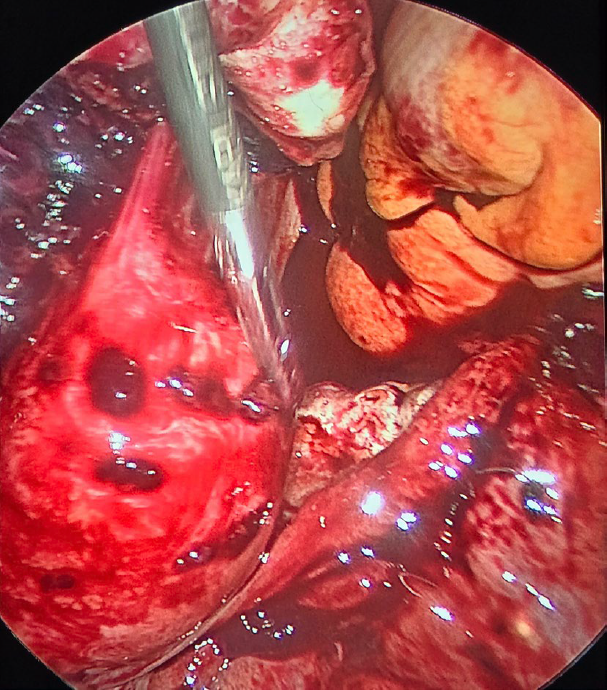
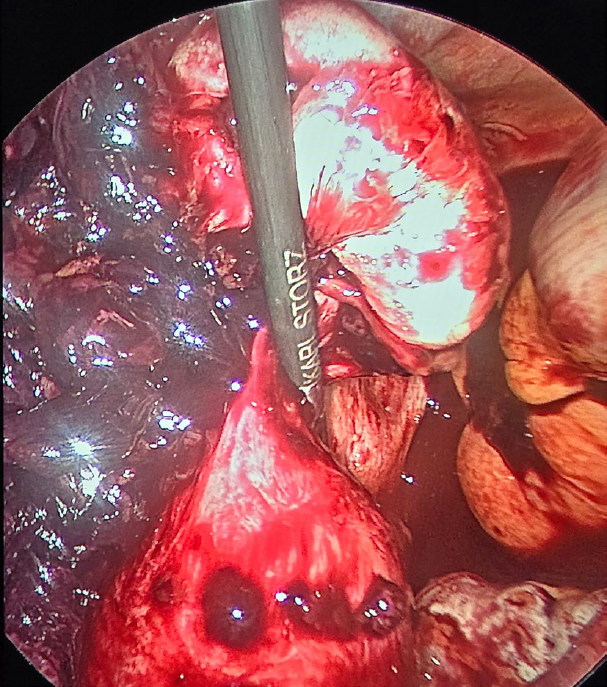
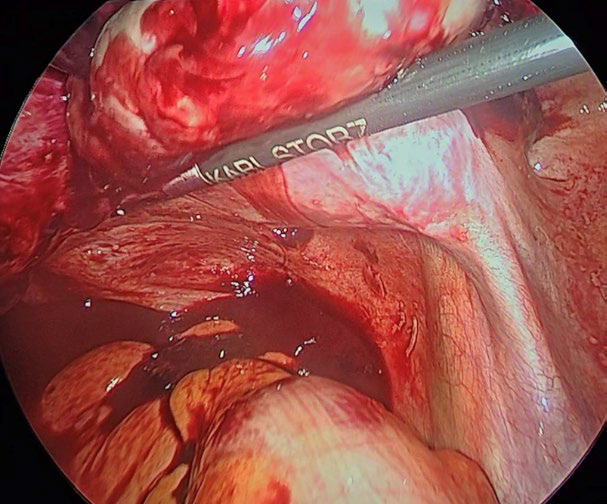
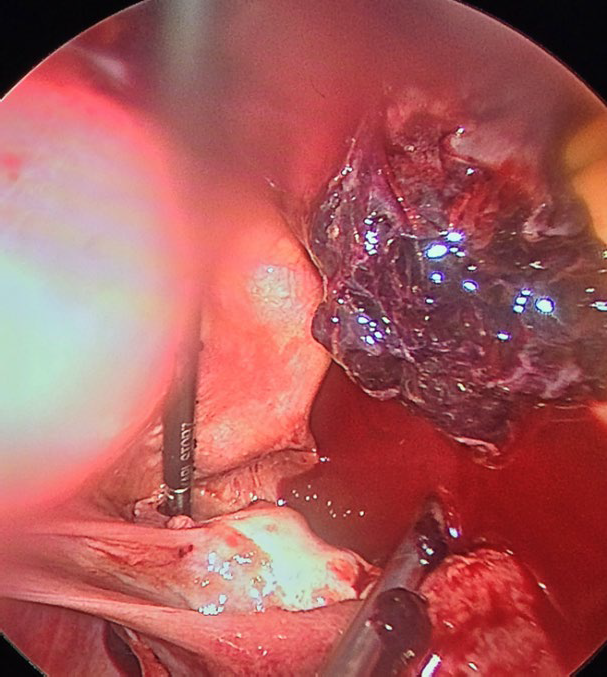
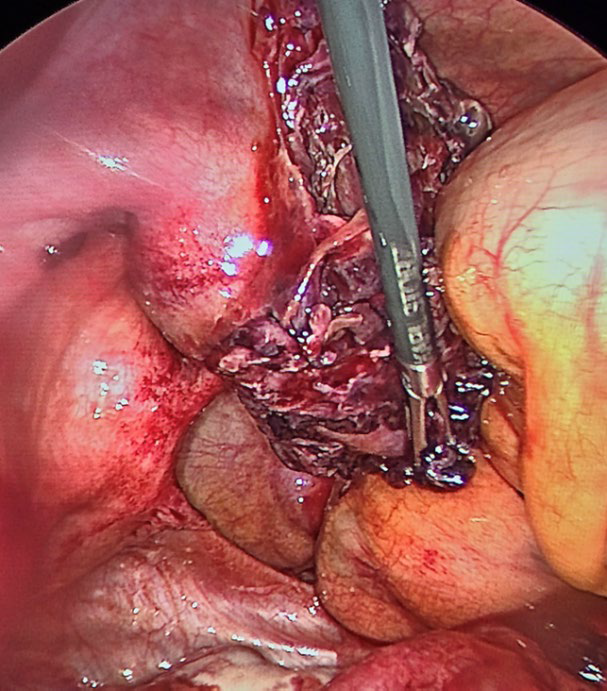
The Gynecological Endoscopy service evaluated the patient and recommended a laparoscopy with salpingostomy to preserve fertility and tubal patency. During surgery, an enlarged uterus was found, with ectopic pregnancy located in the right tube, in the ampullary region, there was a ruptured ectopic pregnancy, measuring 2 x 2 centimeters and associated with a hemoperitoneum of approximately 100 milliliters. A salpingostomy was performed with removal of the embryonic tissue located at the anterior edge of the fallopian tube, using Grasper forceps and a suction and irrigation device. Vasopressin was infiltrated, diluting 20 international units in 100 milliliters of physiological solution, to minimize bleeding. The fallopian tube was then transected to extract the pregnancy using a 5-millimeter trocar, again using the Grasper forceps. In addition, multiple adhesions were identified and released. No intraoperative incidents were reported, as the procedure was performed by a surgeon experienced in minimally invasive surgery. Estimated bleeding during the procedure was 50 milliliters, and the approximate duration of the intervention was 60 minutes. (Figure 1-5).
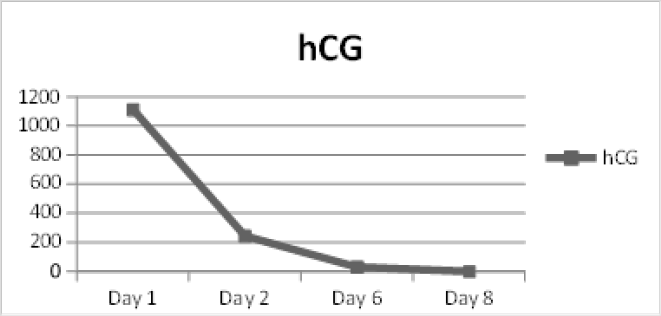
The patient was discharged two days after surgery. During follow-up, laboratory studies showed a rapid decrease in human chorionic gonadotropin levels: 245.1 mIU/mL the next day and 32.29 mIU/mL six days after surgery (figure 6). This case illustrates the benefits of laparoscopic surgery over open surgery, such as a lower risk of complications, less intraoperative bleeding, reduced postoperative pain, and preservation of the fallopian tube, with an adequate decrease in human chorionic gonadotropin levels on the eighth postoperative day, without follow-up ultrasound to check tubal patency.
Discussion
With the development and improvement of laparoscopic technology, the advantages of laparoscopic surgery in the treatment of tubal pregnancy are being clinically recognized. The incidence of tubal pregnancy is gradually increasing and the number of patients with reproductive needs is also increasing, so protecting the reproductive function of patients after treatment has become a critical point. Laparoscopic salpingectomy and salpingostomy are the most common methods for the treatment of ectopic pregnancy.
However, the most viable treatment has been shown to be laparoscopic salpingostomy in order to preserve fertility in patients who wish to retain their reproductive capacity (6), this being a viable therapeutic option due to the skills of the operator (11) and its minimal invasiveness, resulting in an encouraging benefit for the patient (10).
Anatomically, the fallopian tubes are a tubular structure that extends from the horns of the uterus to the ovaries in the female pelvis. It is divided into four parts: the infundibulum, the ampulla, the isthmus and the intramural portion. The ampulla is the widest segment and the most common site of fertilization and implantation of ectopic pregnancies due to its large lumen and highly folded mucosa, which provides a favorable environment for fertilization to occur. The fallopian tubes have an important role in the capture and transport of the egg, as well as in facilitating the meeting between the egg and the sperm. These receive their blood supply mainly through two arteries: tubal arteries and ovarian arteries. The tubal arteries branch from the uterine artery, while the ovarian arteries, which also provide blood supply to the ovary, arise directly from the abdominal aorta. These arteries form a vascular network that ensures adequate blood supply to both the tube and the ovary. The integrity of the utero-ovarian circulation is essential for ovarian function and fertility. (14)
During a laparoscopic salpingostomy, the goal is to remove the ectopic pregnancy from the fallopian tube without removing it completely. This is accomplished by making a small incision in the tube to remove the gestational tissue. Salpingostomy preserves the tubular structure of the tube and, most importantly, the vascular network that connects it to the uterus and ovaries is kept intact, thus preserving blood flow and therefore long-term ovarian function. Which is essential for young women who want to preserve their fertility, since not only the tubal transport capacity of the egg is maintained, but also the hormonal regulation that is vital for reproduction. (3)
In the case presented, the performance of laparoscopic salpingostomy allowed not only the effective elimination of the ectopic pregnancy, but also the conservation of the fallopian tube, thus preserving the patient’s reproductive function by maintaining the tubal anatomy and the utero-ovarian circulation intact.
Also, the rapid decrease in human chorionic gonadotropin (hCG) levels postoperatively was a positive marker that all trophoblastic tissue was successfully removed. During laparoscopy, critical maneuvers such as vasopressin infiltration as a vasoconstrictor agent were performed to control intraoperative bleeding. Vasopressin is injected directly into the serosa of the fallopian tube before the incision is made. This local application causes constriction of blood vessels around the surgical site, significantly reducing blood flow to the area. By decreasing blood supply, vasopressin minimizes blood loss during the removal of gestational tissue, allowing greater visibility for the surgeon and a safer and more controlled intervention. Furthermore, the reduction in bleeding contributes to reducing postoperative complications and improving the patient’s recovery, which is why its administration has proven to be safe and effective during the resection of ectopic pregnancy. (7).
Surgical findings of adhesions in the pelvic cavity were also addressed during the procedure, minimizing the possibility of future complications and improving the anatomical conditions for future pregnancies. Laparoscopic surgery, compared to traditional laparotomy, significantly reduced recovery time, which was reflected in the rapid clinical evolution of the patient (8).
It has been shown that the pregnancy rate after laparoscopic salpingostomy is higher compared to those undergoing salpingectomy, this is because laparoscopic salpingostomy has been shown to better protect ovarian reserve function as well as endocrine function and provide favorable conditions for a second pregnancy, therefore, patients with tubal ectopic pregnancy should give priority to laparoscopic salpingotomy for possibility of pregnancy (9).
The choice of surgical technique should be guided not only by the patient’s hemodynamic stability, but also by her reproductive wishes and intraoperative anatomical evaluation. Laparoscopic salpingostomy, when technically feasible and clinically indicated, offers an excellent option for patients seeking to maintain their fertility while minimizing complications and improving postoperative quality of life (9).
However, conservative management of ectopic pregnancy, like any surgical procedure, is not without risk.
The possibility of a recurrent ectopic pregnancy remains a significant concern for patients who have experienced a previous ectopic pregnancy, especially in the context of conservative surgical techniques such as laparoscopic salpingostomy. This risk not only affects safety in future pregnancies, but also has emotional and psychological implications for patients who wish to conceive again.
According to a published meta-analysis that evaluated fertility outcomes after salpingectomy compared to salpingostomy in patients treated for tubal ectopic pregnancies. In randomized controlled trials, there was no significant difference in the odds of subsequent IUP in patients undergoing salpingectomy compared with those treated with salpingotomy (OR 0.97 CI 0.71-1.33). However, a significant and clinically meaningful difference was observed in cohort studies, in which patients had a lower probability of intrauterine pregnancy after salpingectomy (OR 0.45, CI: 0.39-0.52). With this meta-analysis we found that the probabilities of a repeat ectopic rate favor those patients who were treated with salpingostomy. (15)
Due to the risk of persistent ectopic pregnancy, it is essential to monitor hCG levels after salpingostomy. There are three main methods that use medical treatment, rather than performing a salpingectomy afterwards, due to the risk of PEP after a salpingostomy. The first method involves the routine administration of methotrexate (MTX) prophylactically in all cases, either systemically or locally in the tube; the second is to administer prophylactic MTX only if there are concerns about possible retention or incomplete removal of tissue; and the third is to apply MTX only in women whose hCG levels do not normalize after surgery. (16) Although the outcome in this case was positive, it is essential that further research be conducted on the long-term reproductive outcomes in patients undergoing this type of intervention.
Conclusion
Laparoscopic salpingostomy is considered an effective and preferred technique for the conservative treatment of ectopic pregnancy, especially for patients who wish to preserve their fertility. This procedure not only allows the preservation of the fallopian tube, maintaining ovarian and endocrine function, but also offers the benefits of minimally invasive surgery, such as faster recovery and fewer postoperative complications, as shown in the case of our patient with a good postoperative evolution. However, careful patient selection is essential and rigorous follow-up is essential to optimize long-term reproductive results.
References
Figure 1: Ectopic pregnancy located in the right tube, in the ampullary region, there was a ruptured ectopic pregnancy, measuring 2 x 2 centimeters
Figure 2: salpingostomy was performed with removal of the embryonic tissue located at the anterior edge of the fallopian tube, using a grasper forceps, a suction and an irrigation device
Figure 3: multiple adhesions were identified and released
Fig 4: a hemoperitoneum of approximately 100 milliliters aspirated with 5 mm suction cannula
Fig 5: Incision of the fallopian tube to extract the pregnancy using a 5-millimeter trocar
Figure 6: HCG course day 1 to 8.