Authors / metadata
DOI: 10.36205/trocar5.2024020
Abstract
Study objective: To assess the efficacy of a superior hypogastric nerve modulation in reducing post-surgical pain and additional intake of pain medication after minimally invasivehysterectomy.
Design: Patient blinded randomized controlled trial.
Setting: Multiple hospitals. One surgeon administered the anesthetic in his own surgeries.
Patients: Patients undergoing minimally invasive hysterectomies.
Intervention: Ropivacaine 20ml (0.2%) infiltrated in the retroperitoneal space overlying the superior hypogastric plexus, control of neuromodulation used at the completion of surgery.
Conclusion: The superior hypogastric nerve modulation used during a minimal invasion hysterectomy achieves better post-surgical pain management. It is a simple and effective procedure that any gynecologist with minimal invasion experience can achieve due to its low difficulty level, and low risk.
Introduction
Hysterectomy is one of the most commonly performed gynecologic surgical procedures, with multiple benign indications such as dysfunctional uterine bleeding, endometriosis, and fibroids (1). However, it may also be performed for malignant conditions such as endometrial and cervical cancer in their early stages (2). The hysterectomy itself may be approached by multiple surgical techniques which in simple terms may be classified as minimally invasive (including robotic and laparoscopic approaches), abdominal hysterectomy and vaginal hysterectomy (including laparoscopic-assisted vaginal hysterectomy) (1). There are multiple advantages of the minimal invasión approach in modern gynecologic surgical procedures, such as a noticeable reduction in the amount of postsurgical pain experienced by the patient, earlier recovery and earlier return to he dayto-day routine. There´s also less surgical complications including less case reports of wound infection, fever, sepsis, deep venous embolism, and ileus. Also, minimally invasive hysterectomy may cut the duration of hospitalization to half in comparison to abdominal approach (3). The patient may even benefit from all of the previously mentioned advantages and more, by practicing the enhanced recovery after surgery (ERAS) pathway, which is specifically designed for patients who require any minimally invasive gynecologic surgery, including a hysterectomy. These guidelines are applied during the perioperative period with the purpose of mitigating the physiologic stress response to surgery and promote early recovery. It mainly consists in preoperative patient education, multimodal narcotic-sparing analgesia, nausea, thrombosis and infection prophylaxis, maintenance of euvolemia and liberalization of day-to-day activity (4).
A randomized controlled trial concluded that visceral pain is most significant in the first 24 hours after any surgical procedure. Pelvic visceral pain, specifically, is transmitted through the autonomic nerves, specifically the afferent fibers of the superior hypogastric plexus (SHP). This trial proved that a superior hypogastric plexus neuromodulation (19) reduces opioid medication requirements in the first 24 hours after surgery and is achievable by minimally invasive techniques, including laparoscopy and robot-assisted (5). A retrospective cohort local anesthetic agents in the superior and inferior hypogastric plexus, the post-surgical pain scores given by patients were lower, and it also reduced the use of opioid medication, and helped shortening the time of early post-study showed that after the infiltration of surgical mobilization, favoring earlier discharge (6). Anatomy and Physiology of the Superior Hypogastric Plexus The superior hypogastric plexus, which is the continuation of the upper and lower mesenteric plexus, comes from the preaortic plexus, contains purely sympathetic nerves and is located at the level of the aortic bifurcation, over the sacral promontory. Caudally, this plexus then divides into a right and left segment, extending laterally and further down into the lesser pelvis. After the division, splanchnic lumbar nerves integrate the plexus, and contain sympathetic fibers, receiving the name of Inferior Hypogastric Plexus (IHP) which has both sympathetic and parasympathetic fibers (8). However, up to 40% of people present an anatomy variation, and this plexus may be found at the distal portion of the S1 vertebrae. From the lower hypogastric plexus, emerges an anterolateral branch which innervates the uterus and urine bladder, while the posteromedial branch innervates the rectum (9). Superior Hypogastric Plexus Neuromodulation In 1990, Plancarte et al. described the first SHP block guided by fluoroscopy, where they concluded that delivering local anesthetic to the SHP would lower the neoplastic chronic pelvic pain in the post-surgical period (10). Due to this trial, the primary indication for SHP block is visceral pelvic pain secondary to malignancy of the ovary, uterus, cervix, bladder, or rectum in the female patient.
In 2012, there was a Korean case report of a successful inferior hypogastric plexus neuromodulation with a coccygeal transverse approach technique, using lidocaine, bupivacaine and triamcinolone. They noticed that the classic trans-sacral technique had many secondary side effects and risks such as paresthesia, nervous and vascular damage, organ penetration, and postsurgical infection. So they came up with a new approach to this neurolytic technique. (12) Ultrasound-guided SHP block has also been described, in 2016 Gofeld et al., used the ultrasound as an imaging aid to perform an SHP neuromodulation on human cadavers in the supine position. They achieved bilateral spread by injection of the anesthetic by strict midline placement of the needle. (11) Aytuluk described for the first time a laparoscopic SHP neuromodulation in 2019 and concluded that the most efficient anesthetic to be used during this neuromodulation was bupivacaine, in order to reduce post-surgical pain. (13) However, that same year, Clark et. al concluded that even though and SHP block may reduce immediate post-surgical pain, in experience, it did not relieve pain for more than two hours and did not reduce the opioid consumption in the recovery ward. (14)
Materials and Methods
Our main objective was to investigate the effect of a SHP neuromodulation on postsurgical pain in the first 24 hours after a minimally invasive hysterectomy. Our secondary objective was to evaluate the reduction of additional pain medication intake in these patients, including non-steroidal anti-inflammatory drugs (NSAIDs) or opioids. And lastly, our final objective was to reduce the amount of prolonged hospitalization stay. This was a patient-blinded, randomized, multiple-center study that ran from December 2022 to November 2023. The trial required 92 patients that went through a minimal invasion hysterectomy, in order to detect a reduction of post-surgical pain, additional pain medication intake and hospitalization stay. The patients were randomly assigned into the control and trial group using a computerized number generator. The statistical sample size was used to detect a 30% reduction in post-surgical pain, with an efficiency of 80% and a significance level of 5%. The final sample was of 92 patients; 18 patients in the control group and 74 patients in the neuromodulation group. Participants were required to read and sign their written consent about the possibility of mixed anesthesia procedures that may be used before and after the surgical procedures, as well as their possible side effects: neuraxial injection, discitis, intraosseous injection, intravascular injection or intra-abdominal organ puncture (13, 15, 16, 17). The surgeon who administered de SHP neuromodulation remained a constant during the whole study and has over 10 years of experience in minimally invasive gynecologic surgery, including both laparoscopic and robot-assisted procedures. The surgeon, and the anesthesiologists who prepared the dosage for the SHP neuromodulation, as well as the rest of the theater staff were not blinded to the intervention, however the patients and the recovery nursing staff were unaware of the intervention.
The recruitment included patients who were undergoing laparoscopic hysterectomy for any benign indication. Patients with squamous intraepithelial lesión (I-III) were also considered for this study, and all of them presented a pathology report negative for malignancy. Patients needed to be aged above 18 years and be able to give informed written consent. The only exclusion criteria were allergy to the local anesthetic being used during the SHP neuromodulation (Ropivacaine). After recruitment and consent, baseline data was collected from the patient’s digital file. Further data was collected intraoperatively, including procedure duration, blood loss and any possible complications or incidents during the procedure that may alter the results. All the patients in this trial received general anesthesia before the surgical procedure. (Table 1).
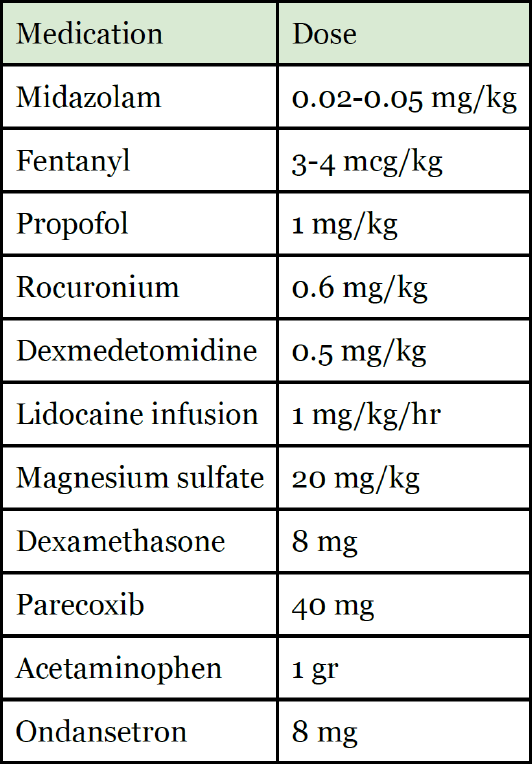
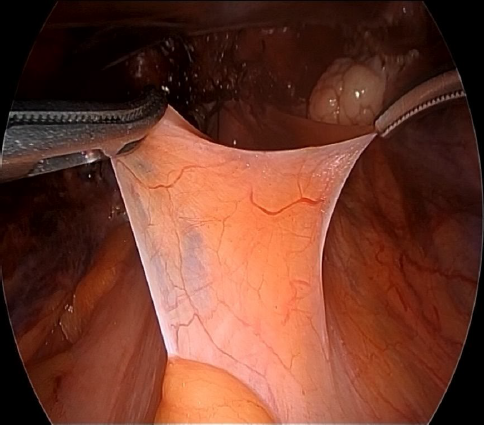
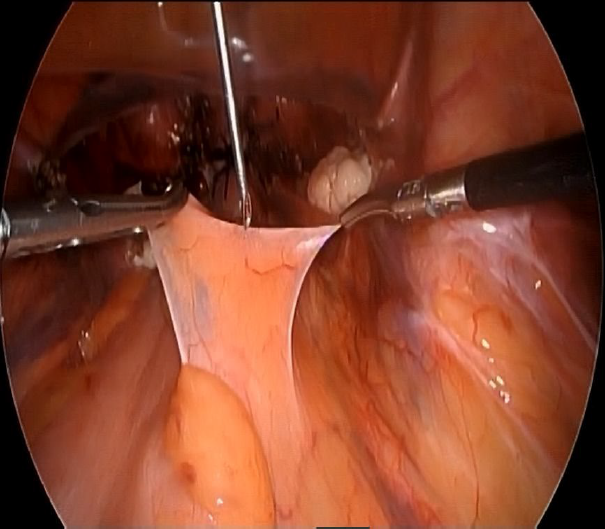
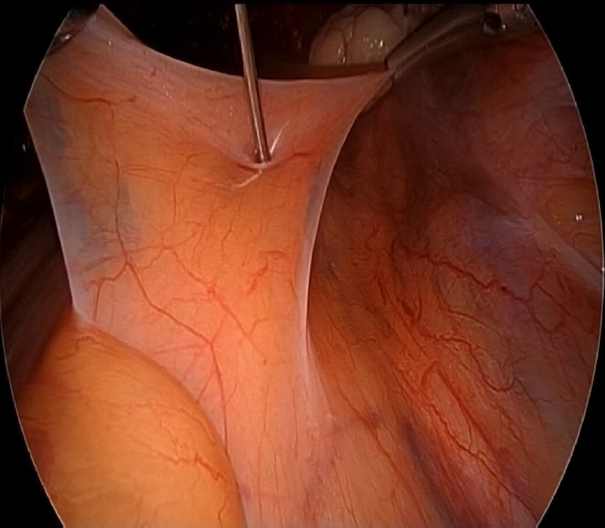
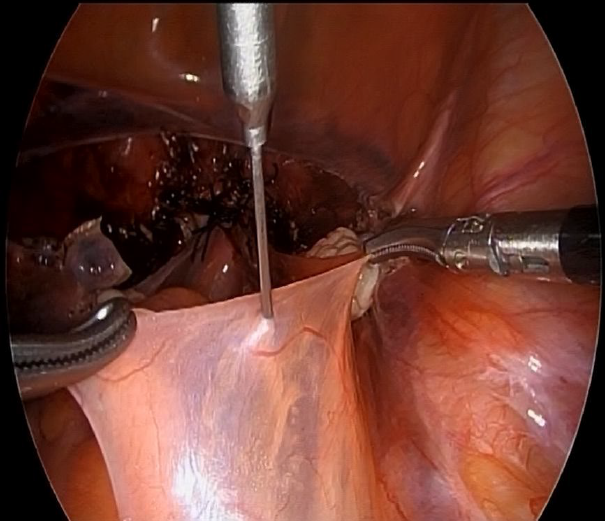
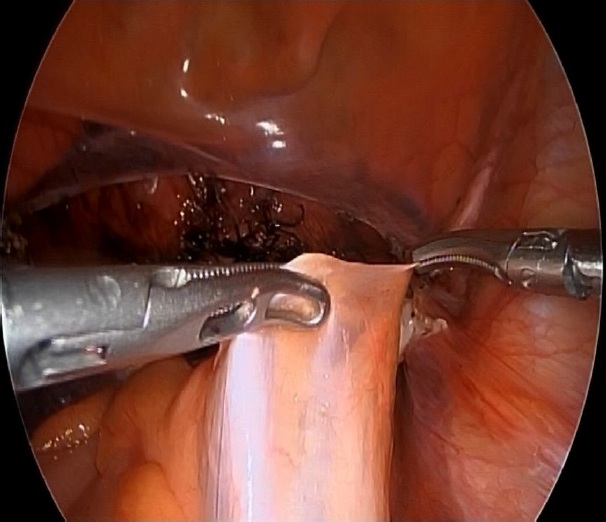
Two lateral 5 mm trocar and one 10 mm suprapubic trocar were needed in all of the procedures. Once the hysterectomy concluded, the patient remained in Lloyd-Davis position, the promontorium was located, and the surgeon managed to arrange the colon to the left in order to get a direct visión of the peritoneum. To administer the medication, two Croce Olmi forceps were used to grasp the peritoneum and tent it up (Figure 1), this way a laparoscopic needle was introduced through the central trocar loaded with ropivacaine 20 mL (0.2%) (Figure 2) and the anesthetic was infiltrated in the retroperitoneal space with the help of the forceps (Figure 3-4). After the withdrawal of the laparoscopic needle from the retroperitoneal space, the Croce Olmi forceps were used to keep the retroperitoneum tented and allow the anesthetic to properly infiltrate the retroperitoneal space (Figure 5). This procedure was performed under direct laparoscopic vision at the end of the surgical procedure, right before the withdrawal of the laparoscopic instruments. This was done with the intention of not letting the surgical time be a biased element that may vary from patient to patient, decreasing the anesthetic effect during the post-surgical period. The anesthetic was successfully administered in all of the patients in the SHP group. There were no immediate complications reported in any of the procedures. Table 1. Medications and doses used to induce general anesthesia and additional medications administered by the anesthesiology team.
After the surgical procedure, we evaluated the effectiveness of the anesthetics during the first 24 hrs of post-surgical care in the recovery ward. We measured the pain using the visual analogue scale of pain, where the lowest score (0) meant painless, and the highest score (10) meant unbearable pain (7). Lastly, we registered the number of times the patient asked the nursing staff for additional pain medication, whether those may be opioids or NSAIDs, and logged the patients that requested an additional day of hospital stay due to pain. All of the patients were given 24 hours of postsurgical stay in the recovery ward. Patients were then discharged with oral NSAIDs and antibiotics, and scheduled for a general checkup 1 and 2 weeks later.
Results
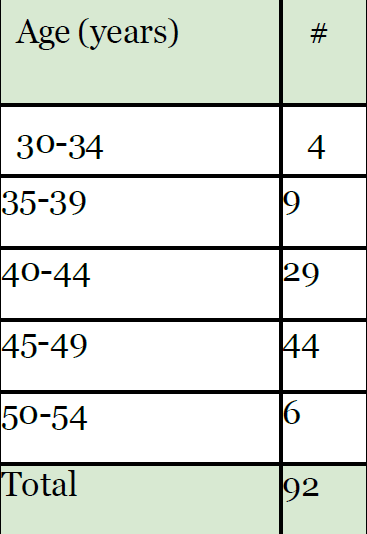
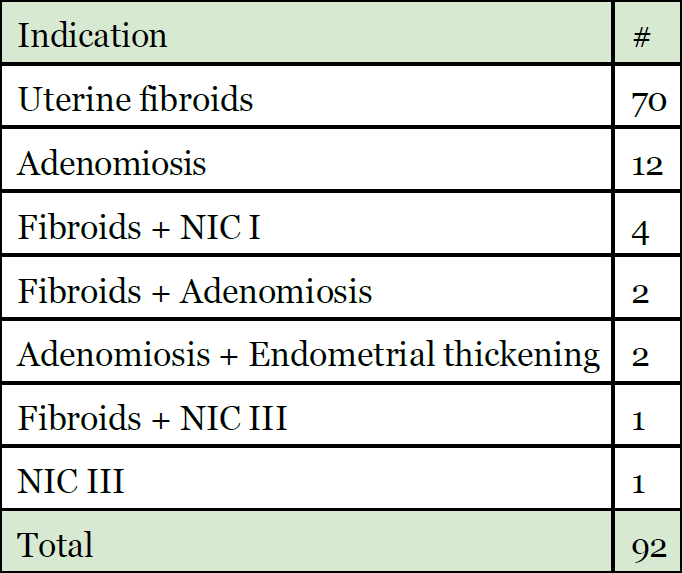
In order to control possible variable outcomes, we did a stratification based on age and the main indication for the hysterectomy. The mean age of the patients who participated in this trial was 44.3 years (Table 2). And the most common indication for the hysterectomy during this trial was uterine fibroids, whether it may be as the only indication, or mixed with other benign or early stage maligns indications (Table 3).
Out of the 92 patients, 74 of them (80%) made up the SHP neuromodulation group and the other 18 patients (20%) only received the standard general anesthesia and intravenous acetaminophen during the first 24 hours after the surgical procedure. During these first 24 hours, 4 patients (3 from the control group (3%) and only one from the SHBP group (1%)) asked for additional painkillers during their stay in the recovery ward. However, no patients (from either group) required opioids or additional hospital stay due to additional pain management. The post surgical pain referred by the patients and the need of additional painkillers was statistically significantly lower in the SHP neuromodulation group, at an average of 2.88 in the pain scale with a standard deviation of 0.79, from 4.11 to 3.87 in comparison to the control group (p<0.05). Meanwhile, the control group reported an average of 4.11 in the pain scale with a standard deviation of 0.96. The average amount of pain reported by the control group was significantly higher in comparison, and the SD was lower in the neuromodulation group, meaning that the pain scale remained more constant to the mean, in comparison.
We also documented the following secondary effects in the neuromodulation group vs. the control group: nausea (10% vs 12%), hypotension (5% vs. 7%), and perilesional pain (5% vs. 7%). There were no severe complications reported in either group of patients.
Discussion
This trial proved that the post-surgical pain experienced by patients may be lower in those who receive an SHP neuromodulation during their minimal invasion hysterectomy. Since 1990, there are records of the benefits that this neuromodulation can bring to lower the post-surgical pain in gynecologic oncology patients (10) and in 2013 the trans-surgical laparoscopic approach was firstly described (13) without needing alternate imaging aids (10,11). However, the surgical technique used during this trial was different because the laparoscopic needle was introduced through the suprapubic trocar port, instead of directly through the navel as other literature previously stated (13).
There already exists a well-known correlation between the multiple benefits for the patients and the use of the minimally invasive approach in all sorts of surgical procedures, including less post-surgical pain and early recovery (3), however, with the SHP neuromodulation there exists an even better postsurgical pain management that benefits the patient, and less need of addition painkiller medication needed to mitigate the pain, bringing and added economic benefit to both the patient and the surgical center. This is why we recommend that all gynecologists with minimal invasion experience can learn and dominate the SHP neuromodulation in order to offer their patients the least amount of post-surgical pain. Since the SHP doesn’t have any motor fibers (8), this neuromodulation may be done without the fear of an accidental motor block. Ropivacaine is the optimal local anesthesia for this procedure, since it mostly works on the Aδ y C fibers which are in charge of pain perception, and it has close to no effect on the motor fibers (Aβ). Also, it has a longer effect compared to bupivacaine, and it has shown less risks of cardiovascular toxicity and secondary effects on the central nervous system (20). Previous trials that used ultrasound-guided administration of this local anesthesia proved that 20 ml were sufficient to achieve an optimal bilateral spread (11). We recommend doing the SHP neuromodulation at the end of the surgical procedure, so that the surgery duration does not affect the effectiveness of the neuromodulation, and so that the prolonged Trendelemburg position may not cause the cephalic dissemination of the anesthesia.
Since there were no prolonged hospital stays (more than one day) in either of the groups, we were not able to compare the economic benefits in that aspect. However, a short hospital stay is an already known benefit of the minimal invasion approach in any surgical procedure (8,9), so this trial may be replicated in patients who need a laparotomy approach hysterectomy in order to establish a shorter hospital stay benefit, obviously using direct vision to administer the SHP neuromodulation, due to the complications previously stated involving the trans sacral y coccygeal approach.
Conclusion
The superior hypogastric nerve modulation used during a minimal invasion hysterectomy achieves better post-surgical pain management. It is a simple and effective procedure that any gynecologist with minimal invasion experience can achieve due to its low difficulty level, low risk and no need for any complex laparoscopic instruments; it is also a procedure that will not lengthen the surgery, since it can take up to only two minutes to execute. It will benefit the patient by allowing her an early return to her day-to-day activities with the least amount of pain possible.
The technique used during this trial (direct administration through a laparoscopic needle) gives an advantage in comparison to other administration techniques, providing an easy and effective access to the hypogastric plexus, with the least amount of complications in comparison to extracorporeal needles or invasive imaging techniques, making this technique an effective way for every gynecologist with minimal invasion experience to provide a hysterectomy with a lower amount of post-surgical pain and less amount of additional pain killers.
I, corresponding author on behalf of all contributing authors, hereby declare that there is no conflict of interest regarding the publication of this paper.
References
Table 1. Medications and doses used to induce general anesthesia and additional medications administered by the anesthesiology team.
Figure 1. Using a grasper and a Maryland instrument to tent up the retroperitoneum.
Figure 2. Introduction of a laparoscopic needle into the abdominal cavity to administer the anesthetic.
Figure 3. Beginning of the anesthetic infiltration.
Figure 4. End of the anesthetic infiltration.
Figure 5. Keep the retroperitoneum tented in order to allow a proper infiltration
Table 2: Age range
Table 3. Hysterectomy indication