Authors / metadata
DOI: 10.36205/trocar5.2024017
Abstract
Asymptomatic auto amputation of the ovary is an extremely rare event that may be due to torsion or inflammation and usually is diagnosed incidentally. A unique case of a freely detached auto amputated left ovary is reported. A 27-year-old female with primary infertility with endometrioma was recovered for Laparoscopic cystectomy. A freely detached auto-amputated left ovary was encountered. During surgery, the findings were that the left ovary was seen lying on the dome of the bladder and partially retroperitoneal in the space of Retzius. The left ovary was not identified in its normal anatomical position in relation to the infundibulo pelvic ligament and utero-ovarian ligament.
Introduction
Auto amputation of the ovary is very rare. The main pathological event of auto amputation is torsion of a normal ovary or an ovarian cyst followed by infarction of the ligament and necrosis or less commonly infection (1–5). While most of the cases of ovarian torsion present with acute abdomen, it may be asymptomatic or delayed in diagnosis till infarction occurs with chronic torsion and later amputation. It may be diagnosed incidentally during a surgery as in our case or during an ultrasound examination (6–8).
The uniqueness of the present case is that there is no reported incidence in the literature of an auto-amputation of an endometrioma.
Case Report
27-year-old nulligravida presented at the clinic with inability to conceive for two years. Her menstrual cycle was regular with 5-6 days flow but she had dysmenorrhea. Her past medical history was not significant. On pelvic examination, the uterus was normal in size. There was no tenderness in either adnexal region. Workup for primary infertility was done. Her AMH was 3.94. All blood and hormonal investigations were within normal limits. An ultrasonographic examination suggested the presence of 7.0 × 5.6× 6.7 cm size echogenic, large cystic mass in the left adnexal region suggestive of ovarian endometrioma. Cancer antigen (CA) 125 was performed; 33.5U/mL. An MRI scan was carried out and demonstrated a well-defined thick-walled hemorrhagic left ovarian cyst measuring approximately 4.6 × 6.7 × 5.9 cm anterior to uterus. The decision was taken to perform a hystero laparoscopy for infertility evaluation and cystectomy of the left ovarian endometrioma. At Laparoscopy, a huge, smooth, globular mass of approximately 7-8 cm in size situated anterior to uterus in region of bladder and partially retroperitoneal in the space of Retzius was noticed. There was no ligamentous or direct connection with the pelvic organs, including the uterus and adnexae, and there was no apparent blood supply to the tumor by the utero-ovarian nor the infundibulo pelvic ligament.
The mass did not appear necrotic as blood supply was probably taken up from surrounding structures. On further examination, it was noticed that the left ovary was not found in its normal anatomic position i.e. in relation to infundibulo pelvic ligament and utero-ovarian ligament. The uterus and the right adnexa appeared normal. The Retzius space was opened and the mass dissected out of the extraperitoneal space and from the dome of the urinary bladder by blunt and sharp dissection. The mass was removed totally intact without any spillage. It was then put in an endobag, decompressed without any peritoneal spillage. It did contain a chocolate-colored fluid material suggesting of endometrioma. The mass was retrieved in the endobag and the specimen send for histopathological examination. Histopathological features are consistent with endometriotic cyst.
Discussion
Endometriosis is a relatively common gynaecological condition affecting 6-10% of women in the reproductive age group (9,10). It is the presence of endometrium-like tissue, outside the uterine cavity and is usually characterized by chronic pelvic pain and infertility. Risk factors for endometriosis include nulliparity, previous pelvic surgeries, imperforated hymen, cervical stenosis and gynaetresia (11). Several theories have been proposed to explain the pathogenesis of the condition with the most popular theory being the retrograde menstruation. Others are the theory of coelomic metaplasia, the immunologic theory, the Müllerianosis and transplantation theory. Another form of endometriosis is as a pelvic mass with the formation of an endometrioma (11). Endometriomas, commonly referred to as “chocolate cysts” are a common form of endometriosis seen in about 17–44% of endometriosis and refers to cysts of the ovaries associated with ectopic endometrial tissue and containing degraded hemorrhagic content hence the appearance of a chocolate-colored effluent when ruptured (10, 11). It is thought that endometriomas form from deposition of endometrial cells with subsequent invagination of the underlying ovarian cortex. Although the majority of chocolate cysts arise from the ovaries, a significant proportion have been found in other sites including the peritoneum overlying the anterior and posterior cul de sac, within the broad ligament and inguinal canal as well as uterine serosa (12, 13). In addition, these cysts can be bilateral and are usually small to medium in size. However, a few have been reported to grow to very large sizes (14). This case report presents an atypical presentation of chocolate cyst. Firstly, the classical clinical symptoms associated with endometriosis were not present in this patient notably cyclical abdominopelvic pain associated with menstruation. Secondly, the left ovary was auto amputated and was attached to dome of bladder and peritoneum of lower anterior abdominal wall, partially extending into the retropubic space of Retzius. It had probably taken blood supply from surrounding structures as it did not look necrotic.
Interestingly, the ultrasound report was suggestive of ovarian fibroma or endometrioma of left side. The first hypothesis is abnormal embryological migration of the left ovary to the ventral wall along the allantois. However, in the case presented the development of the ovary was normal. A second hypothesis was therefore preferred. The etiopathogenic theory to explain adnexal auto-amputation is the mechanical hypothesis, in which an acute or chronic torsion, disrupting the blood flow, leads to ischemia, then necrosis, followed by auto amputation. This remaining mass is either absorbed or evolves towards an auto-amputated ovary which may adhere to surrounding structures or remains as free-floating peritoneal Mass (15-19). Adnexal torsions are in most cases due to the presence of adnexal masses, ovarian cyst or teratoma, or malformations of tubal or ovarian ligaments with over laxity of adnexae (18,19-21).
Adnexal auto-amputation is mostly reported in neonates, but also during Intrauterine life, secondary to abnormal imaging findings on routine ultrasound examination Showing pelvic mass (15,17,19). In teenagers or adults, this phenomenon is more rarely reported but it may also be under-diagnosed as most patients are asymptomatic (15,18). Furthermore, when symptoms do occur, they are non-specific, and mostly consist of chronic pelvic pain with or without palpable mass at physical examination (15,16,18). Previous history of acute lateralized pelvic pain may contribute to the diagnosis of adnexal auto amputation, as was the case in the patient reported herein who presented undocumented lower back pain initially thought to be renal colic. In some women who do not report any history of pain, an undiagnosed fetal or neonate torsion is possible, because it most likely occurs during these periods (17,18,19). Laparoscopic findings classically describe a pelvic mass, either free floating in peritoneal cavity, either engulfed by the omentum or adherent to surrounding pelvic structures, as in the present case (15,16,19).
References
Fig.1: MRI imaging showing leiomyoma anterior to the cervix and anterior vaginal wall
Fig. 2: Intraoperative picture showing large leiomyoma in retro-public space (Space of Retzius)
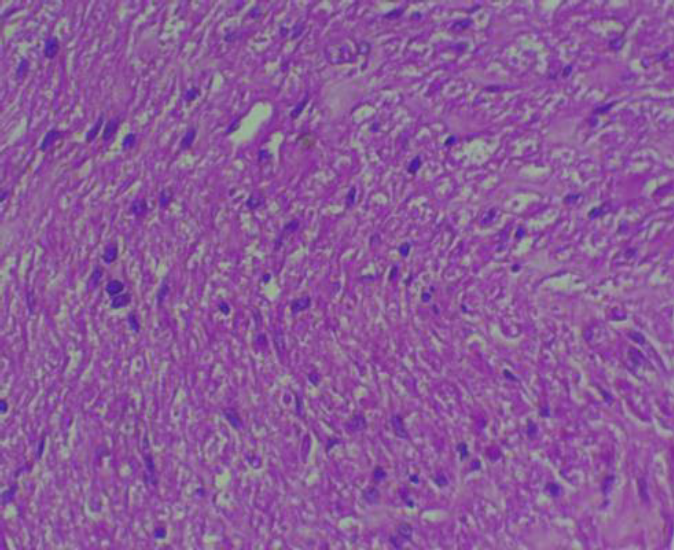
Fig. 3: Histopathology showing leiomyoma cellular pattern similar to uterine leiomyoma
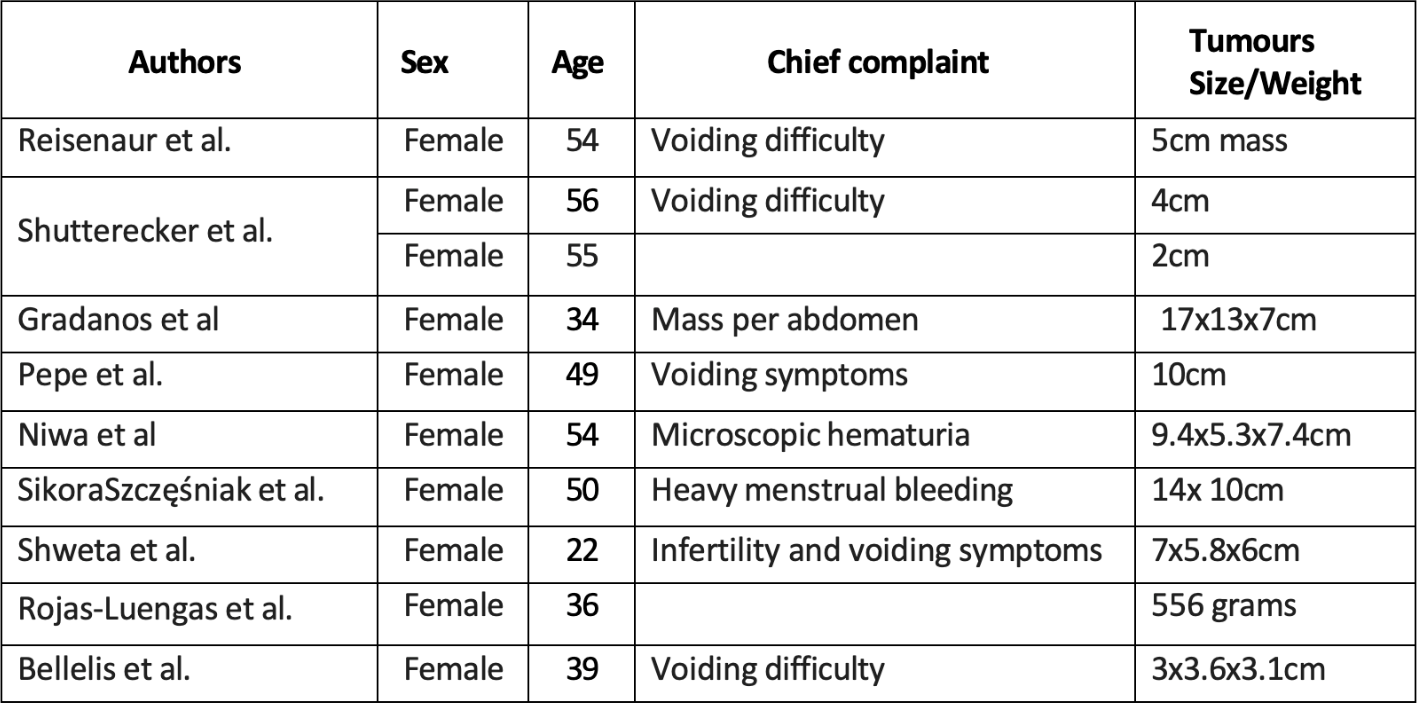
Tab 1. Listing the complaints and tumor size/weight in literature.