Authors / metadata
DOI: 10.36205/trocar5.2024012
Abstract
The treatment of intracavitary pathologies has experienced great progress with the introduction of resectoscopy. In this review, we describe the advances and applications of this technique.
Introduction
In the realm of gynecology, surgical interventions play a pivotal role in managing a myriad of conditions ranging from abnormal uterine bleeding to uterine fibroids and polyps. Among the arsenal of instruments available to gynecologists, the resectoscope stands out as a versatile and indispensable tool for performing minimally invasive procedures within the uterine cavity. This comprehensive review delves into the origins, components, clinical applications, advancements, and future directions of the resectoscope in gynecology.
Origins and Evolution
The resectoscope’s origins can be traced back to the mid-20th century, paralleling its emergence in urological surgery. Pioneers in endoscopic innovations such as Antonin Jean Desormeaux, Gustave Trouvé and Maximilian Carl-Friedrich Nitze laid the groundwork for the development of sophisticated instrumentation capable of visualizing and manipulating the uterine cavity (1). Early iterations of the resectoscope featured rigid designs and limited functionality, necessitating advancements in optics, materials, and instrumentation.
The integration of fiberoptic technology in the 1960s marked a significant milestone in the evolution of the resectoscope, enabling real-time visualization of the uterine cavity and precise tissue manipulation. Subsequent innovations in electrode design, irrigation systems, and electrosurgical energy further refined the resectoscope’s capabilities, transforming it into a cornerstone instrument for gynecological surgery (2).
Continued research and innovation in gynecological surgery have further refined the resectoscope’s design and capabilities, allowing for safer and more effective treatment of various gynecological conditions while reducing the need for invasive procedures. For instance, the “mini-resectoscope” is poised to play a leading role in hysteroscopic surgery for many pathologies, both in inpatient and outpatient settings (3,4).
Components and Functionality
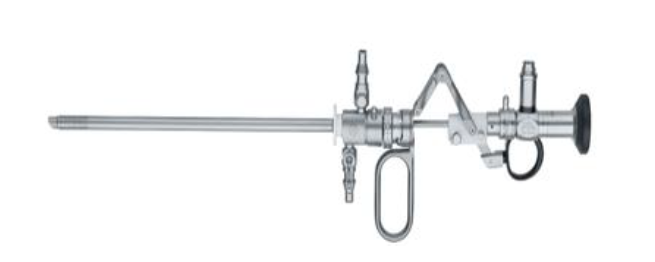
he resectoscope comprises several essential components, each contributing to its functionality and efficacy in gynecological procedures (5).
Sheath: The outer sheath provides structural integrity and houses the working elements of the resectoscope. Constructed from durable materials such as stainless steel or polyethylene, the sheath facilitates smooth insertion into the cervical canal and optimal positioning within the uterine cavity (Fig 1).
Optical System: Central to the resectoscope is its optical system, incorporating lenses and a light source (LED/ XENON) for direct visualization of the uterine cavity. High-resolution imaging enables gynecologists to identify anatomical landmarks, assess lesion morphology, and guide surgical interventions with precision.
Working Elements: The resectoscope features a variety of working elements, including cutting loops, electrodes, and tissue removal devices (Fig 2). These instruments enable gynecologists to perform endometrial resection, myomectomy, polypectomy, and septal resection while minimizing tissue trauma and preserving uterine function.
Irrigation System: Continuous irrigation is essential during resectoscopic procedures to maintain optimal visualization and prevent thermal injury. The resectoscope integrates irrigation ports through which saline or glycine solution is circulated, ensuring clear visualization and efficient tissue dissection (Fig 3). As fluid overload is a main concern with the irrigation systems, newer hysteroscopy pumps have been invented to monitor real-time rate of fluid intravasation (6).
Electrosurgical Generator: Electrosurgical energy is utilized to achieve hemostasis, tissue ablation, and lesion excision during resectoscopic procedures. By modulating power settings and electrode configurations, gynecologists can tailor interventions to patient-specific needs while minimizing the risk of intraoperative complications (7).
Types of resectoscopes
Monopolar Resectoscopes
Monopolar resectoscopes consist of a single electrode that is used for cutting and coagulation. The electrode is connected to a power source, and electric current flows from the electrode through the tissue to a grounding pad placed on the patient’s body.
During surgery, the surgeon uses the monopolar resectoscope to cut and remove tissue, while simultaneously cauterizing blood vessels to minimize bleeding.
This type of resectoscope is effective for procedures such as endometrial ablation and removal of uterine fibroids.
Bipolar Resectoscopes
Bipolar resectoscopes feature two electrodes that are close together, allowing for the passage of electric current only between them. This reduces the risk of damage to surrounding tissue compared to monopolar resectoscopes. The electric current passes directly between the two electrodes, effectively cutting and coagulating tissue in the surgical field without the need for a grounding pad (8). Bipolar resectoscopes are particularly suitable for delicate procedures within the uterus, such as removing polyps or treating abnormal uterine bleeding (9).
Hysteroscopic Resectoscopes
Hysteroscopic resectoscopes are designed specifically for accessing and operating within the uterine cavity (10). There are two types of hysteroscopic resectoscopes- conventional Resectoscope and Mini Resectoscope,
The conventional hysteroscopic resectoscope is a surgical instrument used in hysteroscopy procedures to remove abnormal growths or tissue from the uterus. It typically consists of a long, slender tube with a camera and light source at one end, allowing the surgeon to visualize the inside of the uterus, and a wire loop or other cutting tool at the other end for excising tissue. A conventional hysteroscopic resectoscope typically has a diameter ranging from 15 Fr to 26 Fr.
Mini Resectoscopes
The notable absence of inner and outer sheaths in the Princess Resectoscope underscores its innovative design, diverging from conventional resectoscopes. This streamlined configuration eliminates the need for sheath manipulation, mitigating potential mechanical intricacies inherent in traditional models. By eschewing this dual-sheath structure, the Princess Resectoscope optimizes procedural fluidity, facilitating enhanced maneuverability within the uterine cavity. This technical refinement not only streamlines surgical navigation but also contributes to heightened precision and procedural efficacy, ultimately elevating patient outcomes.
A mini hysteroscopic resectoscope usually has a diameter ranging from 16Fr-22Fr (Fig 4).
Clinical Applications
The versatility of the resectoscope extends across a spectrum of gynecological conditions, offering minimally invasive solutions for patients with uterine pathologies and menstrual disorders:
Endometrial Ablation/ Transcervical resection of endometrium (TCRE): Endometrial ablation using the resectoscope represents a definitive treatment for menorrhagia, or excessive menstrual bleeding, refractory to conservative management. Through thermal or mechanical ablation techniques, gynecologists achieve endometrial destruction, alleviating menstrual symptoms and improving quality of life (11).
Transcervical resection of the endometrium (TCRE) is a surgical procedure used to treat abnormal uterine bleeding caused by conditions such as endometrial hyperplasia or submucosal fibroids. It involves the removal of the endometrial lining of the uterus using a specialized instrument called a resectoscope. Here’s a detailed overview of the TCRE procedure using a resectoscope (12).
Preparation
Before the procedure, the patient may undergo a thorough evaluation, including a pelvic exam, ultrasound, and endometrial biopsy, to determine the underlying cause of abnormal uterine bleeding.
The patient may receive general or regional anesthesia, depending on the surgeon’s preference and the patient’s medical history.
Positioning
The patient is typically positioned on a gynecological table in a lithotomy position, similar to that used during a pelvic exam or childbirth. Stirrups support the patient’s legs, allowing optimal access to the vaginal canal and cervix.
Vaginoscopy: The hysteroscopy is inserted through the vagina initially to look for vaginal pathologies.
Cervical Dilation
The cervix is dilated using a series of dilators or with the assistance of medications to facilitate the passage of the resectoscope into the uterine cavity. Though this step is crucial for ensuring adequate access to the endometrial lining it might not be required in all the procedures.
Insertion of the Resectoscope
The resectoscope is a specialized instrument consisting of a long, slender tube with a light source, camera, and an electrical cutting and coagulation system.
The surgeon inserts the resectoscope through the dilated cervix and advances it into the uterine cavity under direct visualization using the camera.
Visualization and Resection
Once the resectoscope is in position, the surgeon begins to visualize the inside of the uterus on a monitor connected to the camera.
Using the cutting and coagulation electrodes on the resectoscope, the surgeon removes the endometrial tissue layer by layer. The electrical current supplied to the electrodes helps to cut through the tissue while simultaneously cauterizing blood vessels to minimize bleeding. The surgeon carefully maneuvers the resectoscope to ensure complete removal of the abnormal endometrial tissue while avoiding damage to the surrounding healthy tissue.
Irrigation
Throughout the procedure, a fluid (usually a sterile saline solution in case of bipolar resection) is continuously circulated through the resectoscope to maintain a clear field of vision, wash away debris, and prevent overheating of the instrument.
Monitoring and Completion
The surgeon closely monitors the progress of the procedure and ensures that the entire endometrial lining is adequately resected. Once the resection is complete, the resectoscope is carefully removed from the uterus, and any remaining tissue fragments or debris may be flushed out with irrigation fluid or may require removal using ovum forceps in cases of larger chunks.
Recovery
After the procedure, the patient is monitored in a recovery area to ensure stability and to manage any discomfort or bleeding. Most patients can return home the same day or after a short observation period, although some may require overnight hospitalization depending on individual factors.
TCRE using a resectoscope is an effective treatment option for women with abnormal uterine bleeding, offering the advantages of minimal invasiveness, rapid recovery in many cases and preservation of fertility in few cases of superficial TCRE where the basal layer of the endometrium remains intact and undisturbed.
Myomectomy: In cases of symptomatic uterine fibroids, the resectoscope facilitates transcervical myomectomy, a minimally invasive alternative to traditional abdominal surgery. By dissecting and excising fibroid tissue within the uterine cavity, gynecologists preserve uterine integrity and fertility while minimizing postoperative morbidity. Hysteroscopic myomectomy is a minimally invasive surgical procedure aimed at removing uterine fibroids while preserving the uterus. Several techniques are employed in this procedure, including slicing, hydromassage, and variations such as the Metzón and Hamid techniques.
Slicing method: This technique involves using a loop electrode attached to a hysteroscopic resectoscope to slice the fibroid into smaller fragments for removal. The loop electrode is energized with an electrical current, which simultaneously cuts and cauterizes the tissue. The surgeon maneuvers the resectoscope to penetrate the fibroid and create slices, gradually reducing its size until it can be removed through the hysteroscope. This method allows for precise removal of fibroids while minimizing damage to surrounding healthy tissue (13).
Hydromassage: Hydromassage utilizes a combination of fluid irrigation and mechanical cutting to break down and remove fibroid tissue. After accessing the uterine cavity with the hysteroscope and resectoscope, a distention fluid, typically saline solution at bipolar resectoscopy, is introduced to distend the cavity and is alternated with closing the inlet of the fluid whilst aspiration continues. In this way the uterine myometrium contracts and tries to expulse the myoma towards the uterine cavity and facilitate visualization. A specialized device, such as a morcellator, is then inserted through the resectoscope. The morcellator features rotating or reciprocing blades that break the fibroid into smaller fragments. Simultaneously, suction is applied to remove the fragmented tissue from the uterine cavity. This technique is particularly useful for removing larger fibroids or fibroids with irregular shapes (14).
Metzón technique: Named after Dr. Gustavo Metzón, this technique involves using a hysteroscopic resectoscope equipped with a bipolar electrode. The fibroid is dissected and removed using bipolar energy, allowing for simultaneous cutting and coagulation of tissue. The bipolar electrode generates an electrical current that flows only between its tips, minimizing the risk of injury to surrounding structures.
Hamid technique: Named after Dr. Tahar Ben Hamid, the Hamid technique involves using a hysteroscopic resectoscope equipped with a monopolar electrode. The fibroid is dissected and removed using monopolar energy, allowing for precise cutting and coagulation of tissue. A non-conductive distension medium such as glycine solution is required to complete the electrical circuit and deliver energy to the tissue.
Overall, hysteroscopic myomectomy offers several advantages over traditional open surgery, including shorter recovery times, reduced risk of complications, and preservation of fertility. The choice of technique depends on factors such as the size, location, and characteristics of the fibroids, as well as the surgeon’s experience and preference. These advanced techniques allow for the effective treatment of uterine fibroids while minimizing patient discomfort and promoting faster recovery.
Septal Resection: Uterine septa, congenital anomalies characterized by intrauterine partitioning, may predispose to recurrent pregnancy loss and obstetric complications. Utilizing the resectoscope, gynecologists perform septal resection, restoring uterine morphology and enhancing fertility potential for women desiring pregnancy. The resection process requires meticulous attention to detail to ensure the preservation of healthy uterine tissue and to minimize the risk of complications such as excessive bleeding or perforation of the uterine wall.
Polypectomy: Endometrial polyps, benign growths arising from the endometrium, may cause abnormal uterine bleeding and infertility. With the resectoscope, gynecologists can perform polypectomy, removing polyps and restoring the endometrial cavity to optimize reproductive outcomes and alleviate symptomatic burden.
Excision of scar ectopic: Excision of caesarean scar ectopic pregnancy using Resectoscope is an alternative to laparoscopy in certain selected cases and have proved to be an equally effective method.
Isthmocoele repair: Correction of isthmocele using a resectoscope involves accessing the uterine cavity, visualizing the isthmocele, and carefully resecting the tissue forming the defect. This minimally invasive procedure aims to alleviate symptoms such as abnormal bleeding and pelvic pain, with the potential to improve fertility outcomes.
Evacuation of RPOC: In cases of chronic retained products of conception (RPOC), where conventional treatments like medication or dilation and curettage (D&C) have been ineffective, evacuation using a resectoscope offers a minimally invasive alternative. The resectoscope allows for precise visualization and removal of the persistent tissue, reducing the risk of complications and improving patient outcomes, particularly in cases where RPOC have been present for an extended period.
Clinical Considerations and Advancements
While resectoscopic surgery offers numerous benefits, careful patient selection, procedural expertise, and meticulous technique are paramount to optimizing surgical outcomes and minimizing complications. Intraoperative monitoring, fluid management, and adherence to evidence-based protocols mitigate risks such as fluid overload, thermal injury, and uterine perforation.
Recent advancements in resectoscopic technology have expanded the horizons of gynecological surgery, offering enhanced precision, safety, and patient satisfaction. Innovations such as bipolar energy, 3D imaging, and hysteroscopic morcellation have streamlined surgical workflows, reduced operative times, and broadened the scope of resectoscopic interventions.
Gynecological resectoscopes offer several advantages in the diagnosis and treatment of various intrauterine pathologies and conditions. Here are some of the key advantages:
Minimally Invasive: Resectoscopic procedures are minimally invasive compared to traditional open surgeries. They involve inserting a slender instrument through the cervix into the uterus, minimizing the need for large incisions and reducing trauma to surrounding tissues.
Preservation of Uterine Anatomy: Resectoscopic procedures allow surgeons to preserve the structural integrity of the uterus while addressing intrauterine abnormalities such as polyps, fibroids, or adhesions. This is particularly beneficial for women who wish to maintain their fertility or avoid more invasive surgical interventions.
High Precision and Accuracy: Resectoscopes provide high-definition visualization of the uterine cavity, allowing surgeons to accurately diagnose and target specific areas of pathology. The instruments attached to the resectoscope enable precise excision, ablation, or removal of abnormal tissue while minimizing damage to healthy surrounding tissue.
Versatility: Gynecological resectoscopes are versatile instruments that can be used for a variety of diagnostic and therapeutic procedures within the uterus. They are suitable for hysteroscopic examinations, endometrial biopsies, removal of polyps and fibroids, treatment of abnormal uterine bleeding, and management of intrauterine adhesions.
Reduced Recovery Time: Resectoscopic procedures typically result in shorter recovery times and less postoperative pain compared to traditional open surgeries. Many patients can return to their normal activities within a few days after the procedure, leading to improved overall patient satisfaction and quality of life.
Outpatient or Same-Day Surgery: In many cases, resectoscopic procedures can be performed on an outpatient basis or as same-day surgery, eliminating the need for overnight hospitalization and reducing healthcare costs.
Minimal Scarring: Because resectoscopic procedures involve small incisions or no external incisions at all, they result in minimal scarring compared to open surgeries. This can have aesthetic benefits for patients and reduce the risk of complications associated with wound healing.
Effective Treatment Outcomes: Resectoscopic procedures have been shown to be highly effective in treating various gynecological conditions, including abnormal uterine bleeding, uterine polyps, submucosal fibroids, and intrauterine adhesions. They offer durable and long-lasting results with low rates of recurrence in many cases.
Disadvantages
While the resectoscope is a valuable tool in gynecology, it also comes with certain disadvantages and limitations. Here are some of the disadvantages associated with the use of resectoscopes in gynecology (15,16):
Invasive Nature: The insertion of a resectoscope into the uterus requires, although not always, cervical dilation, which can cause discomfort and potential complications such as cervical trauma or uterine perforation, especially in patients with cervical stenosis or anatomical abnormalities.
Risk of Complications: Like any surgical procedure, resectoscopy carries inherent risks, including bleeding, infection, injury to surrounding organs, and fluid overload from irrigation. These risks are generally low but can occur, particularly in complex or lengthy procedures.
Fluid overload is one of the most dreaded complications.
Fluid overload during hysteroscopy occurs when there is excessive absorption or retention of the irrigation fluid used to distend the uterine cavity for visualization. Here’s an overview of fluid overload in hysteroscopy, including its complications, signs, symptoms, diagnosis, and management.
Complications
Fluid overload can lead to hyponatremia, electrolyte imbalances, fluid overload syndrome, and in severe cases, pulmonary edema or cardiovascular collapse (17).
Other complications may include uterine perforation,
Signs and Symptoms:Signs of fluid overload may include hypertension, tachycardia, dyspnea, and peripheral edema. Symptoms can range from mild discomfort to severe respiratory distress, depending on the extent of fluid absorption.
Diagnosis: Diagnosis is primarily clinical, based on signs and symptoms observed during or after the procedure. Laboratory tests may reveal electrolyte imbalances, particularly hyponatremia.
Management
Immediate cessation of the procedure and removal of the hysteroscope to prevent further fluid absorption (18). Supportive measures such as oxygen supplementation and intravenous fluids may be administered as needed. Monitoring of vital signs, electrolyte levels, and fluid balance to assess the severity of the condition. In severe cases, diuretics may be administered to promote fluid excretion, and inotropic agents may be considered to support cardiovascular function. If pulmonary edema develops, respiratory support and close monitoring in an intensive care setting may be necessary.
Prevention is key: using appropriate irrigation fluid volumes, maintaining proper monitoring during the procedure, and promptly addressing any signs of fluid overload can help prevent complications. Overall, prompt recognition and management of fluid overload are essential in hysteroscopy to minimize the risk of complications and ensure patient safety. Close monitoring of patients undergoing hysteroscopy, along with adherence to established safety protocols, can help mitigate the risk of fluid overload and its associated complications.
Limited Accessibility: Resectoscopy may not be suitable for all patients or all types of uterine abnormalities. For example, large or deeply embedded fibroids may be challenging to remove using a resectoscope, necessitating alternative surgical approaches.
Potential for Residual Tissue: Complete removal of abnormal tissue during resectoscopy may be challenging, leading to the potential for residual tissue or incomplete treatment of underlying conditions. This could necessitate additional procedures or interventions in some cases.
Postoperative Symptoms: Patients may experience postoperative symptoms such as cramping, vaginal bleeding, and discharge following resectoscopic procedures. While these symptoms are usually temporary and resolve with time, they can cause discomfort and anxiety for some patients.
Limited Visualization: Despite advancements in technology, the visualization provided by resectoscopes may be limited in certain cases, especially in the presence of significant bleeding or obscured anatomy. Inadequate visualization can compromise the surgeon’s ability to perform precise and effective interventions.
Skill and Training Requirements: Performing resectoscopic procedures requires specialized training and expertise. Surgeons must be proficient in hysteroscopic techniques, instrument manipulation, and management of intraoperative complications to ensure optimal outcomes and minimize risks to patients.
Cost and Resource Intensity: Acquiring and maintaining resectoscopic equipment, as well as providing appropriate infrastructure and support staff, can be resource-intensive for healthcare facilities. Additionally, the cost of resectoscopic procedures may be higher compared to alternative treatment modalities.
Conclusion: Despite these disadvantages, resectoscopy remains an important tool in the armamentarium of gynecological surgeons for the diagnosis and treatment of various intrauterine pathologies. As technology continues to advance and surgical techniques evolve, efforts are ongoing to address these limitations and improve patient outcomes in gynecological resectoscopic procedures.
Future Directions
Looking ahead, the future of resectoscopic surgery in gynecology is characterized by innovation, collaboration, and patient-centered care. Integration of artificial intelligence algorithms for image analysis, predictive modeling, and surgical planning holds potential to enhance diagnostic accuracy, treatment efficacy, and procedural efficiency.
Moreover, the paradigm of personalized medicine underscores the importance of tailored treatment strategies, shared decision-making, and holistic approaches to women’s health. From the emergence of targeted drug therapies to the refinement of fertility-sparing interventions, the resectoscope remains at the forefront of transformative advancements in gynecological surgery.
In conclusion, the resectoscope epitomizes the intersection of technology, innovation, and clinical excellence within the field of gynecology. From its humble origins to its contemporary applications, the resectoscope continues to redefine the boundaries of minimally invasive surgery, empowering gynecologists and improving the lives of women worldwide. As we navigate the complexities of 21st-century healthcare, the legacy of the resectoscope endures as a beacon of hope, progress, and healing for generations to come.
Conclusion
Overall, the advantages of gynecological resectoscopes make them valuable management of intrauterine disorders, offering patients minimally invasive treatment options with excellent outcomes.
Furthermore, the integration of adjunctive therapies such as intrauterine devices (IUDs), pharmacological agents, and regenerative techniques holds promise for optimizing postoperative outcomes and minimizing disease recurrence. From levonorgestrel-releasing IUDs for endometrial protection to platelet-rich plasma (PRP) for endometrial regeneration, the armamentarium of resectoscopic interventions continues to evolve in tandem with scientific advances and clinical insights.