Authors / metadata
DOI: 10.36205/ trocar5.2024009
Abstract
Objective: To evaluate the IBS safety and efficacy as hysteroscopic tissue mechanical removal system for endometrial polyps’ treatment.
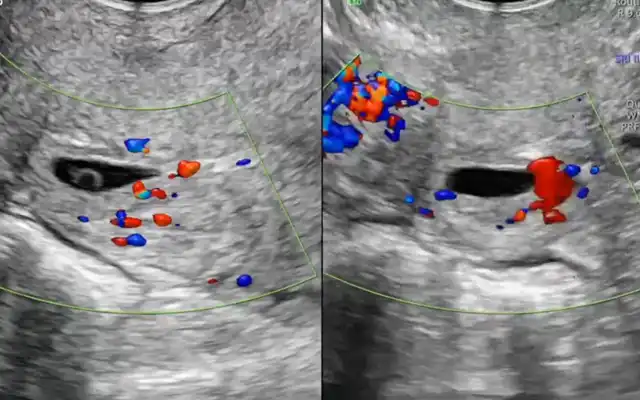
Methods: This retrospective cohort study included 1000 patients with a diagnosis of endometrial polyps carried out at Renji hospital affiliated to Shanghai Jiao Tong University between June 2019 and January 2021. The diagnosis of endometrial polyp was suspected at 2D transvaginal ultrasound and confirmed by a diagnostic hysteroscopy with the Campo Trophyscope. Only patients with polyps larger than 1 cm were included in the study. All patients were treated with the 24Fr. IBS. The recurrence rate was evaluated by 2D ultrasound after 12-month from the operation and confirmed by diagnostic and operative hysteroscopy.
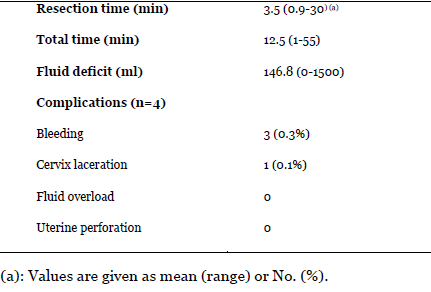
Results: Patients’ mean age was 47.8 years (range 22-86) with a mean childbirth rate of 1.2 (range 0-7). 284 (28.4%) patients were postmenopausal, 324 (32.4%) patients had abnormal uterine bleeding and 266 (26.6%) infertility. The mean operation time was 12.5 min (range 1-55 min) with a mean fluid deficit of 146.8 mL (range 0-1500 mL). Four complications were reported of which three (0.3%) were intraoperative bleedings and one (0.1%) was a cervical laceration during dilatation. No major complication, such as fluid overload or uterine perforation occurred. Only 3 (0.3%) cases were diagnosed of polyps’ recurrence by ultrasound and confirmed by diagnostic hysteroscopy at a 12-month follow up and underwent to a second operative procedure.
Conclusion: This study shows that polyp’s removal with the IBS® is a very safe and precise hysteroscopic treatment. The additional removal of the functional endometrial layer does not result in adhesion formation or post operative complications but in a very low recurrence rate of polyps at 12-month follow-up.
Introduction
Endometrial polyps are the most common cause of abnormal uterine bleeding, and their removal is essential due to their association with infertility and potential malignant transformation [1]. Diagnostic hysteroscopy has shown that 16.5–26.5% of women with unexplained infertility are diagnosed with endometrial polyps [2]. The estimated incidence of malignancy in these polyps ranges from 0.5 to 4.8% [3]. Currently, hysteroscopy is considered the gold standard procedure for treating polyps due to its direct visualization and high accuracy [4]. The bipolar resectoscope, despite its high complication rate, remains the most widely used device for operative hysteroscopy [5-8].
There has been an important technical improvement for polyp’s treatment with the development of hysteroscopic mechanical tissue removal systems [9]. The IBS was specifically designed to enhance efficacy and to reduce the complication rate associated with conventional resectoscopy. By enabling simultaneous removal of tissue chips during resection, the IBS technique provides clear visualization throughout the entire procedure and shortens the learning curve for surgeons [10,11]. This study represents the first large cohort analysis to evaluate the IBS technique safety and efficacy for the treatment of endometrial polyps.
Materials and methods
Study Design
This retrospective observational cohort analysis was conducted from June 2019 to January 2021, at the Sino European Life Expert Centre “SELEC” of RenjI Hospital in Shanghai. Helsinki declaration and Renji Hospital Guidelines were carefully followed in this study [12]. Due to the observational nature of the research, no need of the moral committee approval was required. All patients’ data were anonymized.
Patients
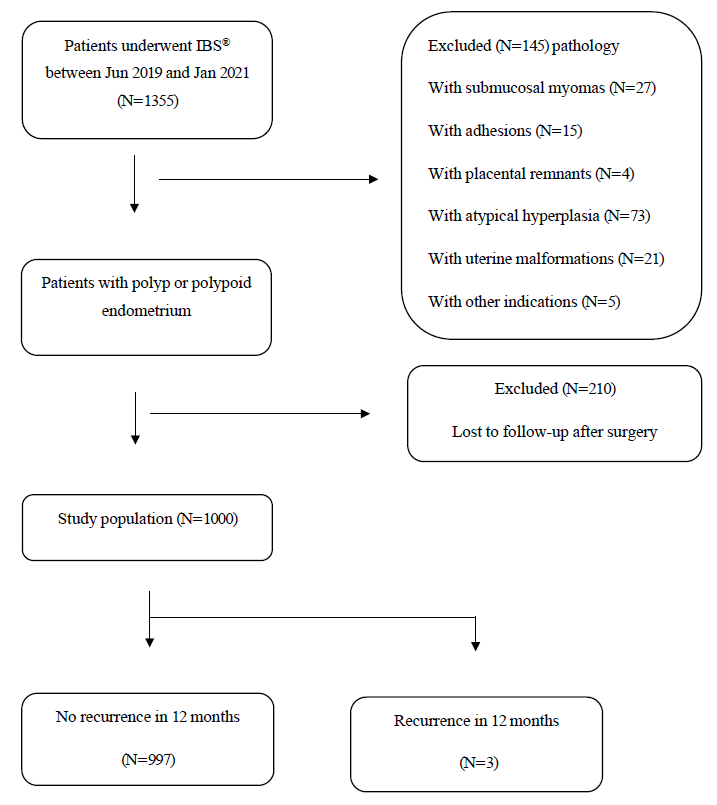
1355 patients undergoing an IBS® hysteroscopic procedure from June 2019 to January 2021 were included in the present study. Of this group, 27 (2.0%) with submucosal myomas, 15 (1.1%) with adhesions, 4 (0.1%) with placental remnants, 73 (5.4%) with atypical hyperplasia, 21 (1.5%) with uterine malformations and T-shaped like uterus and 5 (0.4%) patients with other indications for a total of 145 patients were excluded from this study. 210 patients with the diagnosis of benign polyp were lost at follow-up after surgery and therefore were excluded. The histopathological diagnosis of polyp or polypoid endometrium was confirmed by two different pathologists [1].A total of 1000 patients were included in our survey, including 11 patients with polyp recurrence who underwent hysteroscopic polypectomy before. All patients completed a 12-month, follow-up survey. Personal medical history, resection time, operation time, and complications were recorded. For total operation time we considered the time of the whole procedure. On the other hand, we considered the resection time as the time from the view of the shaver tip inside the uterine cavity until the end of resection.
Equipment
All polypectomies were performed with the 24Fr. IBS® (Karl Storz SE & Co. KG Tuttlingen Germany). A detailed description of the equipment was presented in our previous publication [10]. The diagnostic and office hysteroscopies were performed with the Campo Trophy scope® (Karl Storz SE & Co. KG Tuttlingen Germany).
Surgical Procedure
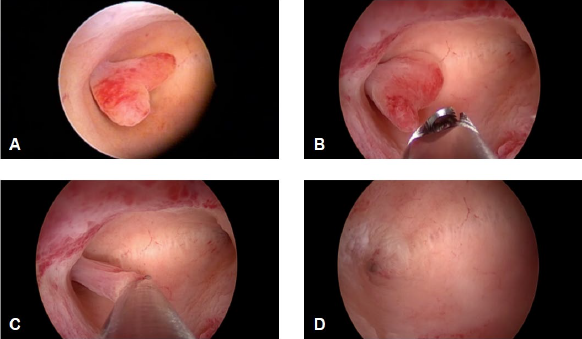
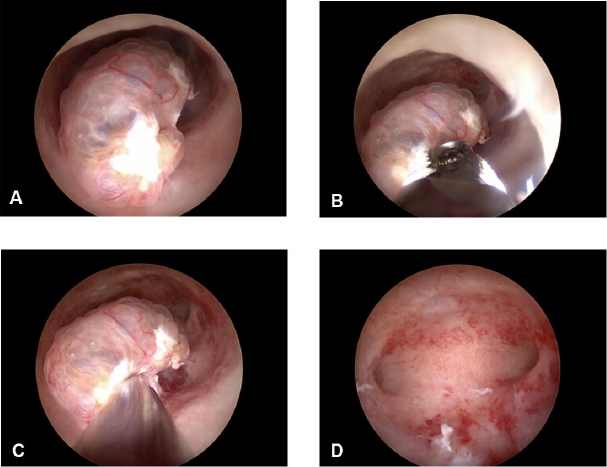
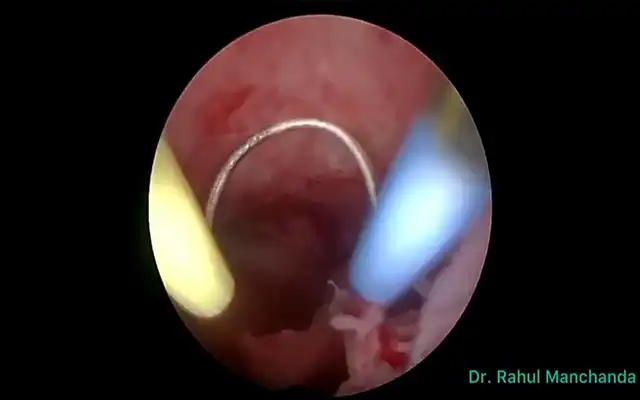
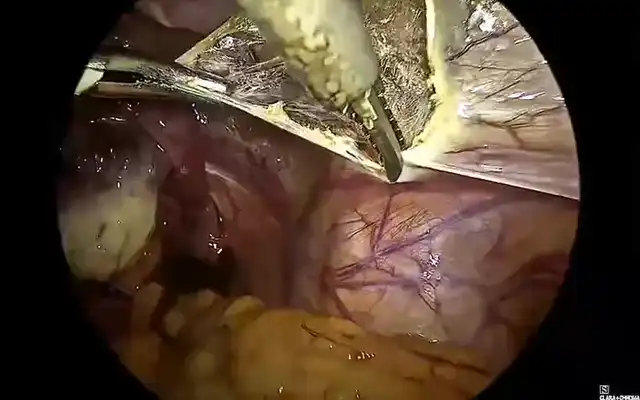
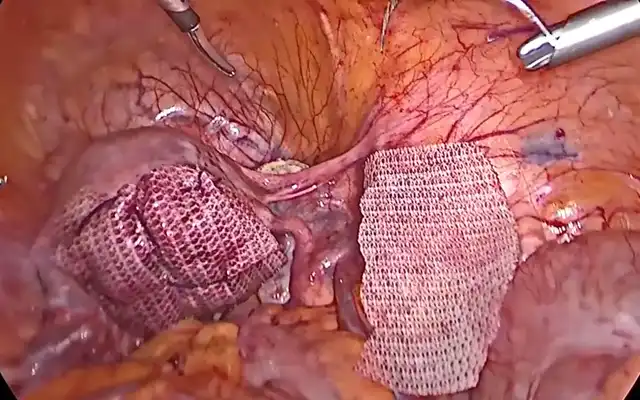
All operations were performed under general anaesthesia, and a standard gynaecological set up was used in all operating theatres. After cervical dilatation up to number 8.5 mm of Hegar, the IBS® 24Fr. optics was inserted inside the uterine cavity. Once the pathological site was exposed and visualized, the rigid shaving system connected to the motor drive unit was inserted inside the operative channel and the polyp’s resection could begin. The rotating oscillating movements of the inner blade of the shaving system cut the tissue allowing specimen aspiration for histology. We used an IBS® oscillating rotation power of 2100 RPM with an aspiration flow of 250ml/min (Fig.1-2). Polyps were removed starting from their edge until reaching their base. In all patients the polyp’s removal was extended to all the functional endometrial layer to improve both symptom relief and pregnancy outcome. All treatments were performed by expert surgeons with similar educational background and surgical skill in the IBS® use. Both 19Fr. and 15 Fr. IBS® were not yet available in China during our study and therefore general anaesthesia, due to the large diameter of the 24 Fr. IBS® optics, was necessary.
Data Collection and Follow-up
Dr Xia Yin and Xiaoshi Liu retrospectively collected all data from the patients’ clinical charts (recorded at time of polypectomy). All patients completed a 12-month follow-up survey and were contacted by telephone to evaluate patients’ symptom improvements and to retrieve missing information. All patients regularly received a transvaginal ultrasound and were seen at periodic gynaecological office examination every six months to assess polyp recurrence.
Results
Patient cohort
From June 2019 to January 2021, 1355, patients underwent IBS® hysteroscopic procedures at the Sino European Life Expert Centre, RenJi Hospital of Shanghai. Patients were included in the study if two pathologists confirmed the histological diagnosis of polyp or polypoid endometrium. Among this group, 27 patients (2.0%) had submucous myomas, 15 patients (1.1%) had adhesions, 4 patients (0.1%) had placental remnants, 73 patients (5.4%) had atypical hyperplasia, 21 patients (1.5%) had uterine malformations and T-shaped uterus, and 5 patients (0.4%) had other indications for a total of 145 exclusions from the study. Additionally, 210 patients diagnosed with benign polyp were lost to follow-up after surgery and were therefore excluded from this study. Finally, a total of 1000 patients were included in our survey. All the patients underwent transvaginal ultrasound followed by diagnostic hysteroscopy with Campo Trophy scope® before the Operative Hysteroscopy. Polyps larger than 1 cm were included In the study as polyps with a lower diameter were directly removed during the office procedure. Eleven patients had undergone hysteroscopic polypectomy before our IBS® operation, and polyp recurrence was found during their follow-up. A total of 1583 endometrial polyps were completely removed during operative hysteroscopy (Fig.3). During each surgical procedure, one to five polyps were removed. The basic clinical characteristics of the 1000 patients are summarized in Table1.
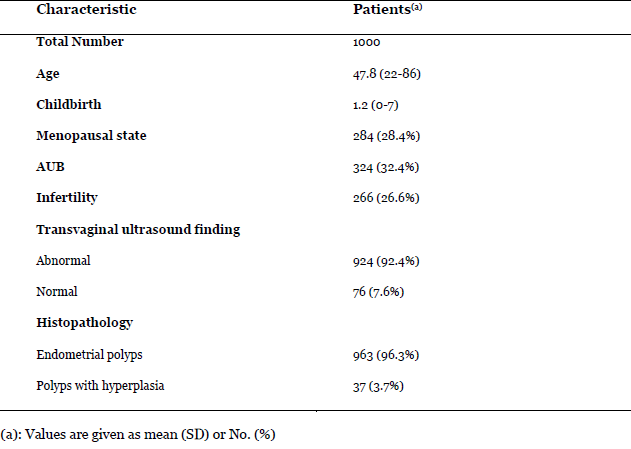
The median age of patients undergoing treatment was 47.8 years (ranging from 22 to 86 years) and mean childbirth was 1.2 (range 0-7). There were 284 (28.4%) women in thepostmenopausal state, with a mean age of63.2 years. In 324 (32.4%) patients and in266 (26.6%) the indication for operativehysteroscopy was abnormal uterine bleedingand infertility respectively. For 963 patients(96.3%) the histopathological diagnosis wasendometrial polyp, while for 37 cases (3.7%)was an association of polyp and hyperplasticendometrium.
Safety and efficacy
The operation time was recorded for all patients, with a mean duration of 12.5 minutes (ranging from 1 to 55 minutes). The mean resection time was 3.5 minutes (ranging from 0.9 to 30 minutes). In this study, the mean of fluid deficit was 146.8 ml (Table 2). A total of four complications (0.4%) were reported. Three cases involved intraoperative bleeding, and one case involved cervical laceration. Intraoperative bleeding was treated with administration of intravenous oxytocin and with the aid of a bipolar probe introduced inside the strait operative channel of the shaver optics during the procedure. No major complications such as fluid overload or uterine perforation were reported. 211 (21.1%) women were treated with oral contraceptives or progesterone for 3-6 cycles to prevent recurrence afterpolypectomy. During the 6 months follow-up, 39 patients were still symptomaticwithout abnormal transvaginal ultrasoundfindings. After completing a median 12-month follow-up, only 3 (0.3%) patients were symptomatic and had a polyp recurrencesuspected at ultrasound and confirmed bydiagnostic hysteroscopy. Eleven patientswho had previous postoperative polyprecurrence did not experience recurrenceagain after the IBS® treatment. There wereno late complications like intrauterineadhesions or hypomenorrhea. The threepatients underwent to a second IBS®operative procedure to remove the recurrentpolyp.
Discussion
Endometrial polyps account for about 80% of endometrial pathology. They represent a focal or diffuse glands and stroma overgrowth of the endometrial functional layer. [13,14]. They can be sessile or pedunculated [13] with a size that ranges from a few millimetres up to several centimetres. Abnormal uterine bleeding is the most common symptom and occurs in 68% of premenopausal and postmenopausal women with endometrial polyps [14,15]. Most endometrial polyps are benign with a possible malignant transformation in 3.2 to 6.7% of cases [16-17]. Hysteroscopic polypectomy using the mechanical tissue removal systems has been shown to be a fast, safe, and well-tolerated technique, with a very short learning curve [9,19] as previously reported by Bigatti et al [20]. Until now, very few large-scale cohort studies to evaluate this procedure have been performed.
The primary endpoint of this study was to assess the IBS® (Karl Storz SE & Co. KG Tuttlingen Germany) safety and efficacy for polypectomy in a retrospective cohort study on a large number of patients. 1000 procedures were included in our study. All polyps were successfully excised with a mean operation time of 12.5 minutes (range 1 from 55 min) and a mean resection time of 3.5 minutes (range 0.9-30 min). Compared to the bipolar resectoscope, surgery was not interrupted by tissue chips removal, which explains the very short operation and resection time. Only normal saline was used with no fluid overload syndrome. Despite uterine perforation is the most common complication at hysteroscopy [21,22,23] none of this damage was reported in our retrospective cohort study. All IBS® procedures were performed under visual control as tissue chips were removed at the same time as resection. The high perforation rate of bipolar resectoscopy is mainly due to the reduced visibility induced by the tissue chips that stay inside the uterine cavity after resection. In addition, the in and out movements performed to remove the tissue chips from the uterine cavity after resection to clear the impaired visibility, increase the overall surgical time with a high risk of fluid overload syndrome, gas embolism and cervical laceration [5]. In our study we reported only 3 (0.3%) cases of intraoperative bleeding, which were all solved with the use of the bipolar probe. The IBS® has already proved to be a valid alternative of bipolar resectoscope.
This benefit is confirmed by a better endometrial layer healing process with a lower risk of uterine rupture and an improved fertility outcome [24-25]. According to several studies, the endometrial polyp recurrence rate ranges from 2.5 percent to 43.6 percent, depending on the length of follow-up and the size of the polyps [27,28]. In our study we have reported an improvement regarding AUB symptoms after polypectomy. Only 3 (0.3%) patients experienced recurrence, requiring further hysteroscopic evaluation, at the 12-month follow-up. 11 patients in our cohort underwent hysteroscopic polypectomy before and found polyp recurrence during their follow-up but none of them experienced recurrence after IBS®-assisted hysteroscopic polypectomy. One possible explanation of this low recurrence rate could be the concomitant removal of most of the functional endometrial layer in fertility age patients. Only 28.4% patients in our cohort were postmenopausal therefore reducing the risk of bias.
Additionally, the absence of patients undergoing hormone replacement therapy in our study could also contribute to the lower recurrence rate. No postoperative adhesions or even Asherman syndrome was reported at follow up as the IBS® action did not involve the basal endometrial layer. All successfully treated cases experienced normal cycles after operative hysteroscopy with the Shaver technique. At present our study is the largest population-based cohort study to evaluate both efficacy and safety of the Shaver technique in case of polypectomy. The findings of this study confirm the validity of the IBS® as a safe and successful method for polyps’ removal. The findings of very low recurrence rate together with the very low complication rate and the short learning curve make this technique as the gold standard procedure in case of endometrial polyps’ treatment.
Author contributions
Conceptualization: RC and GB. Data collection: XY, SZ and JS. Data analysis: XY and XSL. Data management: XY, XSL, AMZ, YW and WD. Manuscript draft: XY and XSL. Manuscript revision and review: YX, XSL and GB. All authors read and approved the final version of the manuscript.
Conflicts of interest
Dr G. Bigatti is a consultant for Karl Storz SE & Co KG Tuttlingen, Germany, and a developer of the IBS® device reports personal fees from Karl Storz SE & Co KG Tuttlingen, Germany outside the submitted work. Dr R. Campo is a consultant for Karl Storz SE & Co KG Tuttlingen, Germany, and a developer of the Campo Trophy Scope® reports personal fees from Karl Storz SE & Co KG outside the submitted work. No support from the financial industry was received for this study.
Acknowledgements
Special thanks are addressed to Prof. Wei Ping Li of the Shanghai Jiao Tong University Affiliated Renji Hospital for his support in the realization of the “SELEC” Sino European Life Expert Centre, and to Dr Rudi Campo of the LIFE Expert Centre of Leuven for his cooperation and advice on the design of this study.
References
Figure 1: IBS® resection of an endometrial pedunculated polyp. A Before; B, C During; D After IBS® treatment, respectively. The polyp is completely excised with respect of the surrounding healthy endometrium.
Figure 2: IBS® resection of an endometrial cystic polyp. A Before; B, C During; D After IBS® treatment, respectively.
Figure 3: The enrolment process
Table 1 Characteristics of the 1000 patients treated with the 24Fr. IBS®.
Table 2 Surgical procedures and complications in patients treated with the 24 Fr. IBS