Authors / metadata
DOI: 10.36205/trocar4.vid20234
Abstract
Submucosal myomas represent 5.5% to 16.6% of all uterine fibroids (1). Several treatment options are available in clinical practice nowadays (2). Bipolar resectoscopy still remains the gold- standard surgical procedure to approach submucosal myomas (3). Fluid overload, uterine perforation and long learning curve are still unsolved, technical related, problems (4). With the advance of new surgical devices an alternative and completely mechanical approach to tissue removal has been developed. Currently there are three main tissue mechanical removal systems: Truclear®, Myosure® and Intrauterine BIGATTI Shaver (IBS®). Despite several advantages, such as shorter operative time, higher total resection rate and higher patient acceptability, myoma size and consistency still limit the use of tissue mechanical system for this indication (5). In 2014 Bigatti et al. reported that the IBS® was able to remove in a single-step procedure 93.5% of submucosal myomas up to 3 cm in diameter, 62.5% of which were type II (6). In 2023 Zhang Shu et al. by reducing the IBS® rotational speed from 2100 rpm to 1500 rpm and increasing the aspiration flow rate up to 500 ml/min achieved a more complete resection and a faster operating time especially for myomas between 3 and 5 cm in diameter (7). This case report shows a two steps procedure with the IBS® for the successful removal of a large 6 cm submucosal degenerated myoma.
Video article
Two – steps procedure with the Intrauterine BIGATTI Shaver (IBS®) for a large, 6 cm degenerated G1 submucosal myoma removal: a case report
Study Objective: To assess the IBS® efficacy for the treatment of a large 6 cm – G1 submucosal myoma.
Design: Description of the surgical steps and prognosis related to this approach. Setting: “SELEC Sino European Life Expert Centre” of JaoTong University, Shanghai Patient:
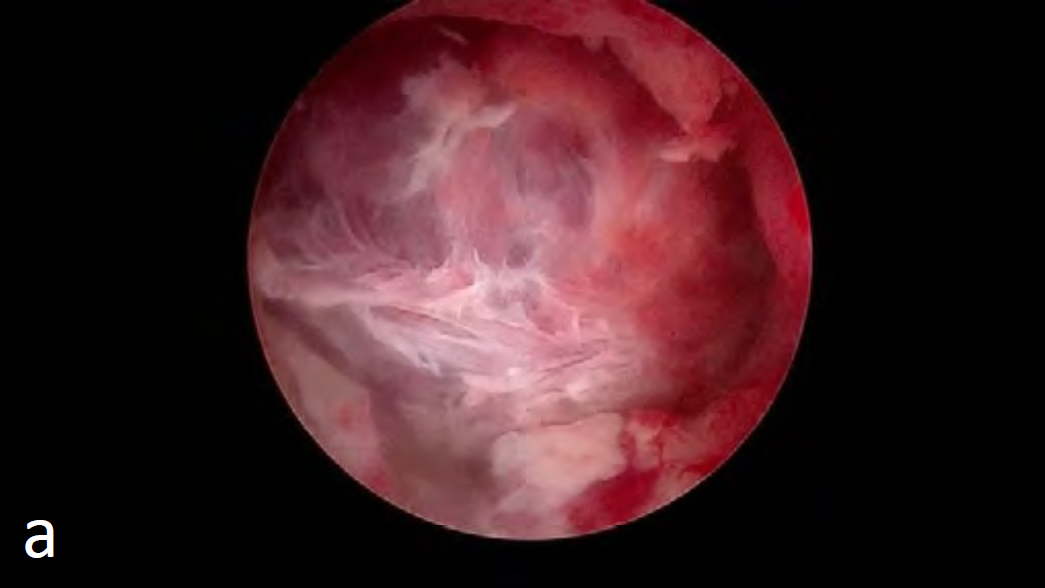
A 27-year-old nullipara woman was admitted to our hospital with a one-year history of abnormal uterine bleeding.On examination, the uterus was enlarged to 10-weeks of pregnancy in size. Her hemoglobin was low at 95g/L with a normal CA125 and Ca19.9 levels. Transvaginal ultrasound showed an 80mm×87mm×96 mm anteverted uterus with a type 1, 55mm×68mm×60mm submucous myoma inside the uterine cavity according to FIGO classification (8). Both ovaries were of normal size. At diagnostic hysteroscopy the presence of a G1submucous myoma almost occupying the whole cavity and inserted into the left side of the uterine fundus was confirmed (9). The red color and the tenderness of the myoma capsule gave us the impression of a partial necrotic degenerated myoma. The vascular patterns on and around the myoma appeared normal and therefore a biopsy of the fibroid prior to removal was not felt to be necessary.
Intervention
An operative hysteroscopy utilizing the IBS® (KARL STORZ SE & Co. KG) was scheduled. The 24Fr. optical system with an SB blade of the shaver was used. A detailed description of the equipment has been published previously (10). The procedure was carried out under general anesthesia and the hysteroscopic distension medium chosen was normal saline. The rotational speed of the blade was set to 1500 rpm with an aspiration flow rate between 250ml/min and 500 ml/min. As described in our previous diagnostic hysteroscopy, the uterine cavity was completely distended by the presence of the G1 myoma with several organized blood clots. A two-stage procedure was required as the fluid deficit limit was reached during resection of the intracavitary portion of the fibroid (Fig.1).
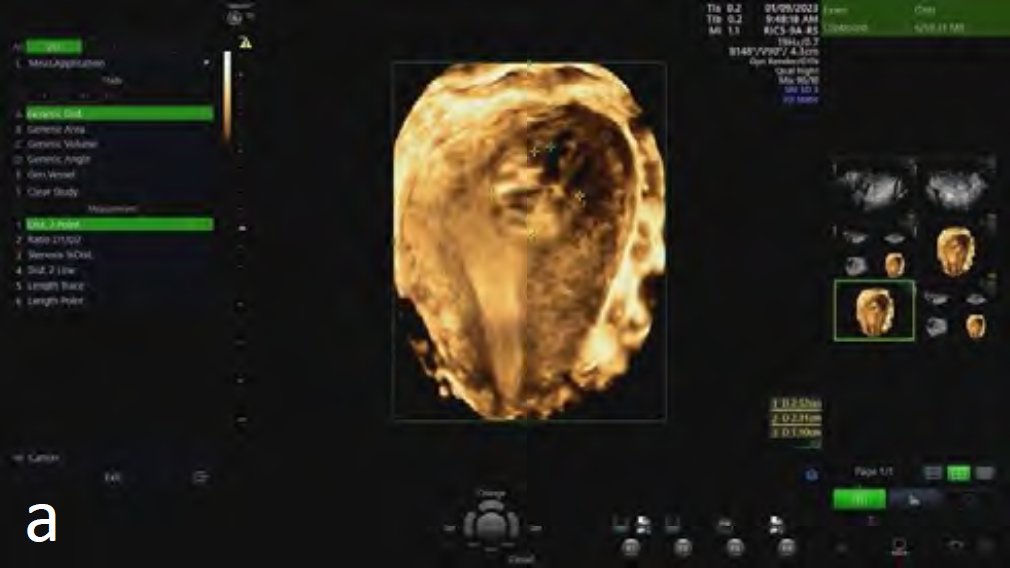
This procedure lasted around 25 minutes but as the fluid deficit reached 2000mL, the decision to stop and reschedule for complete resection at a second stage was taken. The histological examination confirmed the presence of a partial necrotic degenerated submucous myoma. After the first surgery the patient experienced an improvement in her menstrual flow with no more abnormal uterine bleeding. At transvaginal ultrasound two months after surgery a 2.5 cm residual myoma was found. The residual myoma was completely removed at second surgery (Fig.2).
The IBS® was also used with an operative time of 20 minutes and a fluid deficit of 500 ml of normal saline solution. The procedure was almost bloodless with no anesthesia-related complications. To prevent adhesion formation, a Mate-Regen® gel by Bioregen was left in cavity at the end of the procedure. The patient was discharged from the hospital two hours after both operations.
Main result
At a three months postsurgical evaluation the patient reported normal cycles without intermenstrual abnormal uterine bleeding. Transvaginal ultrasound confirmed the completeness of the myoma removal with the presence of a normal endometrial thickness.
Conclusion
The IBS® system has been shown to allow completion of most major operative hysteroscopic procedure in a single step (11,12,13). It has been shown to be precise, safe and with a short learning curve, The shave technique allows the removal of polyps and fibroids without affecting the basal layer and thereby reduces the risk of post-surgical adhesions. Due to its mode of action, electrosurgery which may cause thermal damage is not involved in the process. This is the reason why this technique should be the first choice in case of infertility patients. However, the removal of large submucosal myomas by the IBS® is still a challenging hysteroscopic operation. A rotational speed of 1500 rpm with an increased aspiration rate up to 500 ml/min increased our performance in the removal of intrauterine submucous myomas. This case report confirms the validity of the Shaver technique for this indication and therefore the need to promote further technical research on tissue mechanical removal systems to improve the success rate in case of removal of all kinds of large submucosal myomas.
Conflict of interest: Dr G. Bigatti is a consultant for Karl Storz SE & Co KG and a developer of the IBS® device reports personal fees from Karl Storz SE & Co KG outside the submitted work. No support from the financial industry was received for this study.
Video
References
Figure1: Stage 1 procedure: a) 6 cm degenerated submucosal myoma b) Final image after the removal of the myoma intracavitary portion c) Total amount of tissue removed.
Figure 2: Stage 2 procedure: a) 3D US of the residual Intracavitary portion of the degenerated submucosal myoma b) Final image after the removal of the myoma residual intracavitary portion c)Total amount of tissue removed.