Authors / metadata
DOI: na
Introduction
Over the past 50 years, MIGS has evolved in a relatively short period of time to overtake the centuries-old visionary and pioneering groundwork of our outstanding colleagues in all surgical disciplines. Minimal Invasive Surgery (MIS) began with the innovative approach of Philipp Bozzini who died in 1809 at the age of 36 years. He basically invented the illumination of body cavities using an extracorporeal light source to reflect light. The beginning of Endoscopic Surgery from a surgical perspective starts with Georg Kelling, who presented the first endoscopic procedure, viewing the stomach of a dog, using Nitze’s cystoscope and an air insufflation apparatus at the Natural Scientists’ Meeting in Hamburg, Germany in 1901.
Departed innovative thinkers and visionary mentors, such as Raoul Palmer, Hans Frangenheim, Kurt Semm, Daniel Dargent, Patrick Steptoe, Jordan M. Phillips, Maurice Bruhat, Robert B. Hunt, Jochen Lindemann, Thoralf Schollmeyer, and our general surgical colleague Gerhard Buess, all struggled to introduce less disabling diagnostic and therapeutic endoscopic technologies into daily clinical use for the betterment of our patients [Table 1].
Table 1: Founding fathers of laparoscopic and hysteroscopic surgery
Jacques Hamou, Dennis Querleu, Marc Possover, Frank Löffer, Christopher Sutton, and Harry Reich, the Nezhat brothers, under the lead of Camran Nezhat, – Nargesh Motashaw, Prashant Mangeshikar, Prakash Trivedi , Shailesh Putambekar and Akhil Saxena – under so many Indian and other dedicated colleagues around the world like Ibrahim Alkatout, Joerg Keckstein , Bruno van Herendael, Guenter Noe and Keith Isaacson are contemporary gynecological visionaries whose achievements have set the path which we now follow. The worldwide development and popularization of gynecologic endoscopy and endoscopic surgery in all medical disciplines began when Professor Kurt Semm became chief of the Department of Obstetrics and Gynecology at the University of Kiel, Germany, in 1970. I was then a first year resident in the OB.GYN Department in Kiel, Germany, but had an education of three years in General Surgery in the Amazon Hospital in Pucallpa, Peru, when I joined him. After initial tubal sterilizations in Kiel in 1970, ovarian cyst- resections, ectopic pregnancies, and myomectomies followed and were performed successfully however, sutures and ligatures were difficult to acquire.
Manufacturers were eager to produce only if large quantities of surgical products were ordered. With the introduction of laparoscopic cholecystectomy by Erich Mühe in 1985 and Phillipe Mouret in 1987, industry realized the importance and potential commercial benefits of this endoscopic surgical development and became more interested in endoscopic surgery. There are many milestones in the chronological development of minimal invasive surgery which are very well detailed in our Practical Manual of Laparoscopic and Hysteroscopic Gynecological Surgery (1 and 2). The development of safe coagulation strategies by Kurt Semm and Video laparoscopy with better and better camera systems by Camran Nezhat (USA) set milestones (3).
Many national gynecological endoscopic societies as well as multidisciplinary societies of endoscopic or MIS/medicine (SLS, ITS, and SMIT, ESGE, ISGE, AAGL, APAGE) have since been formed. From 1970 to 1990, gynecological laparoscopic surgery continued to be developed in Kiel under Kurt Semm. Numerous national and international endoscopy courses took place in Kiel, Clermont Ferrand, Brussels, Lyon, Strasbourg, in various locations in the USA and worldwide. In 1990, the Kiel School of Gynecological Endoscopy was founded by Liselotte Mettler and continues today under the leadership of Ibrahim Alkatout. Since 35 years, Prashant Mangeshikar of Mumbai, India, visited this school with annual courses of 30–40 Indian gynecologists and general surgeons for 2 weeks of intensive endoscopic surgery and training. This means dedication and recognition of our Indian colleagues, who today are leading worldwide in their open and critical discussions of surgical endoscopic procedures in modern multimedia.
ISGE, APAGE, ESGE and AAGL direct with their many national and International Endoscopy courses and meetings the world standard in Gynaecological Endoscopic Surgery, whereas. SLS and SMIT support the interdisciplinary cooperation of all medical and surgical specialities
Specifications
Where are we standing today with the Catalogue of Organ-oriented Indications for Operative Laparoscopy/Pelviscopy and Hysteroscopy in Gynecology?
Can all surgical procedures be done endoscopically? (Pelviscopy is the term used by Kurt Semm for Gynecological Laparoscopy).
A variety of operating indications in our field has been established during the past 5 decades, including surgery on the uterus and the adnexa for benign and for malignant reasons. Many patients have benefited from the use of laparoscopy, particularly those with extra uterine pregnancies or endometriosis. Today, the field of endometriosis includes intensive cooperation with general surgeons, especially in the treatment of deep infiltrating endometriosis reaching into the bladder and bowels. There are less complications, shorter hospital stays, and faster rehabilitation. Laparoscopic interventions are now possible for intestinal tumors, female genital tract tumors, adhesiolysis, genital suspension operations, resection of rudimentary uterine horn, incision of lymphocele and during pregnancy. Furthermore, the endoscopic treatment of malignant disorders, including multiorgan procedures such as lymphonodectomies or pelvic exenterations, shows their progress. The very well discussed results of the LACC study brought cervical cancer surgery to acertain halt and reflection. However, newer studies have proofed that early cervical cancer surgery can only be performed laparoscopically in the hands of expert surgeons respecting two principals:
- Application of a cervical vaginal tissue sleevearound the cervical tumor and
- No use ofintrauterine manipulators.
This proofed to havethe same results in cancer progression rates andlong-term survival rates for the patients as opensurgery (4 and 5).
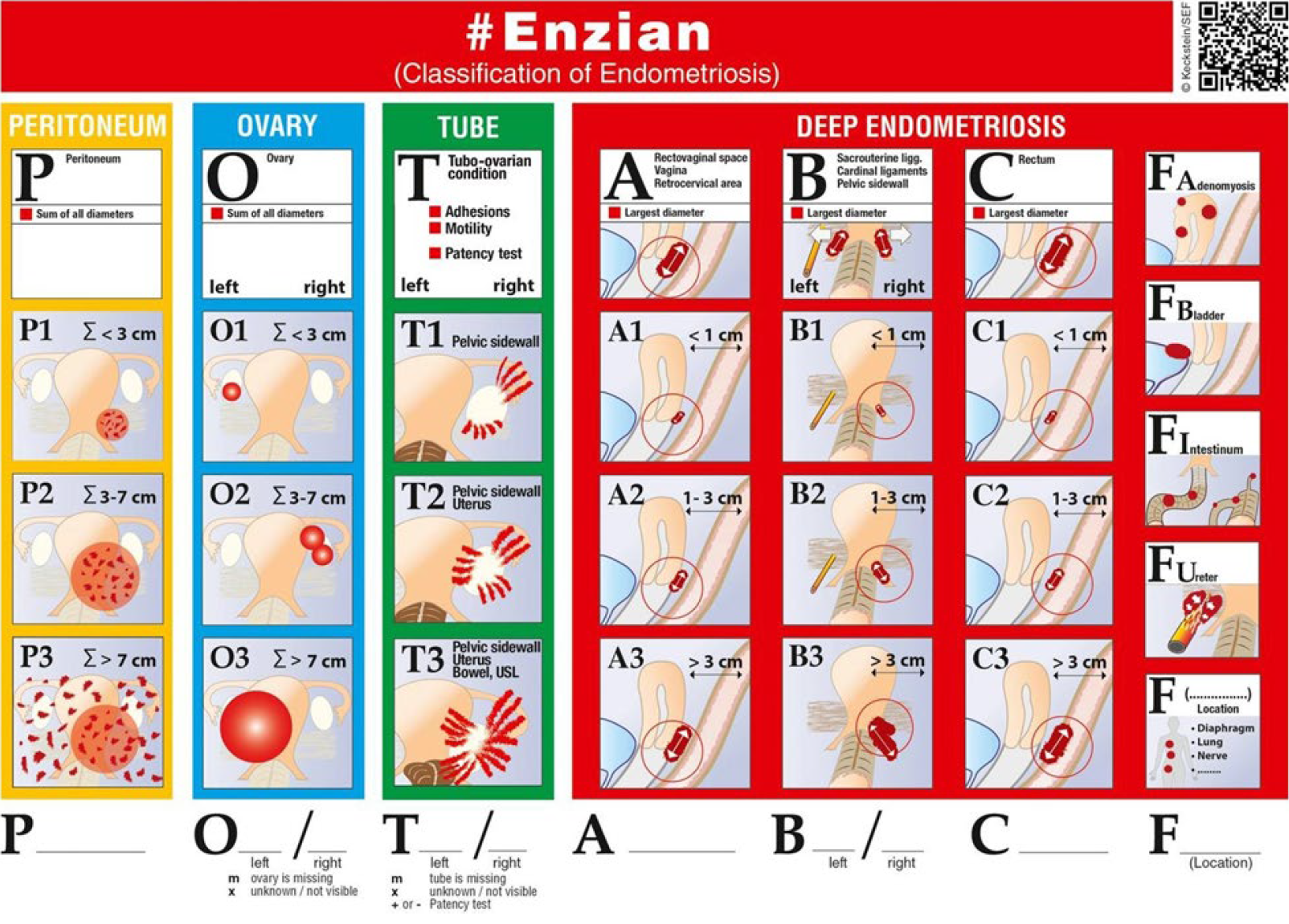
An overview does not permit to go into selected examples of laparoscopic and hysteroscopic surgery, therefore I will only give one example on current endometriosis surgery based on the European #ENZIAN score for ENDOMETRIOSIS as preoperative and postoperative classification (table 2).
Endometriosis surgery has of course improved over the 50 years of laparoscopic diagnosis and treatment. However, histologically, the lesion remains the same. While we all know the endoscopic endometriosis classification (EEC), which we published again in 2006 and again 2017 (6)which is in good accordance with the IFFS,rASRM classifications, the fertility index (endometriosis fertility index [EFI]) and ESHRE classification, we use since 2012 the #Enzian classification [Figure 2]. EEC Stages3 and 4 are further detailed with the #Enzian classification. Recently in Human Reproduction, EQUSUM was published merging the three most frequently used Endometriosis classifications which are: American Society for Reproductive Medicine (rASRM), #Enzian and EFI (6 and 7).
Quality and Safety Issues in Endoscopic Surgery
Although minimally invasive endoscopic surgery was generally pioneered and popularized by gynecologists over the past decades, teaching institutions failed to inspire and invest in endoscopic education and research, with the same enthusiasm and dedication as our general surgical and other colleagues did. Given the prevailing political, educational, industrial, and societal realities while facing most advanced economies, we are destined to grapple with a protracted period of fiscal restraint, consumer demands, and societal expectations.
In Canada, with a relatively small health market (population 34,482,779 million), health expenditure in 2019 was expected to reach $265 billion, although health spending actually decreased in proportionate terms. It was anticipated that, overall, health spending represented 11.5% of Canada’s gross domestic product. Thus, every country has to set a certain amount of money for health and health-related technology aside.
Future Aspects
Goals of Good Surgery are identical whether we perform laparotomy, laparoscopy, vNOTES (vaginal Natural Orifice Transluminal Surgery) or endoscopic conventional or robot assisted procedures, regardless of the angle, location, or means of access:
Let us continue along the path of minimal trauma, maximum vision and good tactile feeling to ensure optimal surgical success until times with protons or other magical bullets open up new options to treat pathologies. It is conceivable that within the near future, pre-operative early recognition of pathological conditions with contemporary imaging technologies – the merger of imaging and endoscopy has already occurred – and better molecular-genetic recognition of disease – the human genome has already been described – will automize or even make extensive radical surgical procedures unnecessary.
We are already experiencing the next generation of genetics and metabolomics (?). These fields will render extensive surgeries unnecessary in the future and we will rely only on minimal invasive surgery which requires three fundamental components: Skilled surgeons or well programmed robotic automated procedures, depending on the input of technical data and measurement together with spontaneous machine recognition = artificial intelligence. Instruments and apparatuses are the key features that enable a skilled surgeon to perform optimal, precise, and indicated surgical procedures with minimal inflammation, adhesions, and complications.
Exchange of knowledge
Thanks to the ready exchange of knowledge between military institutions, aviation, space technology, informatics, engineering, mathematics, biology, genetics, and medicine as well as human dedication to disease exploration, technological advancements are no longer bound in one field. Journals are our present optimal exchange of ideas. Every written article needs special dedication and educates the writer at the same time.
Technical developments
Technological advances with improved endoscopic instruments for hemostasis and non-traumatic procedures as well as suturing skills allow us endless choices and possibilities. Precise, endoscopic, and robotic surgery, most likely preprogrammed with intraoperative imaging will be the only surgical tool in 2050.
Bloodless surgery with articulated and robotic instruments with multiple degrees of liberty and precision coagulation will be possible. Computer-assisted instruments tips will allow the surgeon to position the angles to the desired tissue planes and give tactile feedback.
Conclusion
It must be stressed that the history of laparoscopy and hysteroscopy and its introduction in the surgical practice is a story of many researchers, who for years battled against prevalent general thinking and partly against rejection of their brainchild of performing ‘gentle operations.’ Many of the pioneers were ignored, called dreamers or regarded as crazy. It is only through their persistence, their tenacity, their strong personalities and their intense dedication to life and love, that they could stand firm in the face of adversities. For India let us fully acknowledge the immense input of Shailesh Puntambekar (8) and Meenu Agarwal (9) of Pune, India.
The history of laparoscopy is a unique mixture of various trends in different fields, spurred by the activities of established societies as well as opportunities of their publication and influenced by the world’s progress, recession, war, piece and the love of the individuals for life. The influence of industry, which has kept pace and actively supported this development for years, is the driving force besides the heroes of doctors and engineers that bring up new ideas. Without suitable technology, this dissemination would not have been possible. Endoscopic development and its future does depend on new inventions, on the audacity of leading heroes, their input into this field but also on their management of life to continue to survive on a healthy and successful cooperation with the medical technical industry and the governments of our countries which grant us the freedom of research and development for the best of all our patients.
Today laparoscopic and hysteroscopic surgery represent modern ways of surgery and are on the way to be the leading interventions with least trauma and good surgical outcomes. We have to be open for new technologies as robotic surgery, which is together with artificial intelligence at present – after its 20 years of development – the trend of the time.
Robotic surgery is the most dynamic development in the sector of minimally invasive operations at the present time in 2024. It should not be viewed as an alternative to laparoscopy, but as the next step in a process of technological evolution. The advancement of robotic surgery, in terms of the introduction of the Da Vinci Xi, and other robots on the surgical market, permits the variable use of optical devices in all four trocars. Due to the new geometry of the “patient cart,” an operation can be performed in all spatial directions without re-docking. Longer instruments and the markedly narrower mechanical elements of the “patient cart” provide greater flexibility as well as access similar to those of traditional laparoscopy. Currently, robotic surgery is used for a variety of indications in the treatment of benign gynecological diseases as well as malignant ones. Interdisciplinary cooperation and cooperation over large geographical distances have been rendered possible by telemedicine, and will ensure comprehensive patient care in the future by highly specialized surgery teams. In addition, the second operation console and the operation simulator constitute a new dimension in advanced surgical training. The disadvantages of robotic surgery remain the high costs of acquisition and maintenance as well as the laborious training of medical personnel before they are confident with using the technology, but there are roads in vision to overcome that and let this surgery take over in laparoscopic surgical procedures as the leading technology.