Authors / metadata
DOI : 10.36205/trocar3.2023004
Abstract
Introduction: Tubal obstruction is one of the common causes of female infertility and almost always needs artificial reproductive technology. Anatomical improvement of the tubes using surgical procedure are expected to restore their function. However, it raises the risks, cost, and morbidity. Previous studies show good technical success rates for fallopian tube recanalization (FTR) using minimally invasive transcervical tubal catheterization.
Objectives: To report the outcomes of three cases of infertility due to bilateral non-paten tubes with performed FTR.
Case Operation Procedure: We retrospectively evaluated the three cases of FTR procedures performed from July to November 2022 at Dr. Moewardi Hospital. The three cases had undergone a basic infertility evaluation and established diagnosis of infertility due to bilateral non-patent tubes. Infertility due to anovulatory and male factors were excluded. Minimally invasive transcervical tubal catheterization- hysterosalpingography with high pressure contrast injection followed by fluoroscopy were performed.
The success of the technique was established if both patent tubes were obtained at the end of the procedure. Clinical pregnancy was established if gestational sac obtained on transvaginal sonographic examination within 10 weeks post-procedure.
Discussion: The fallopian tube, as a place of fertilization in the reproductive process, is very dependent on the health of its anatomy and physiological function. In studies of infertility in women, tubal factor infertility is the most common cause of infertility. Case-1 was a five years primary infertility, the technique was successful but patient did not conceive.
Case-2 was a one-year primary infertility, the technique was successful, and patient achieved a spontaneous pregnancy eight weeks after the procedure.
Case-3 was a five years secondary infertility, the technique was successful, but no pregnancy was obtained.
Conclusion: There were three technical successes in the three cases that underwent FTR, one of which became pregnant.
Introduction
Tubal factor infertility is a factor of infertility in women which can be caused by post infection fibrosis, spasm of the tubal ostium, and tubal obstruction. This tubal abnormality can occur at one side of the tube or bilaterally Trisna et al., 2019 (1). Diagnosis of tubal abnormalities can be done to determine tubal patency through laparoscopy to hysterosalpingography (HSG) Hardel et al., 2022 (2). This condition can be corrected by various tubal recanalization procedures under assistance of endoscopy, interventional treatment with radiology, or assisted treatment with traditional Chinese medicine (TCM) Liu et al., 2017 (3). In various studies, interventional radiological procedures are more recommended to be performed because it is minimally invasive and cost-effective with good outcome Mohan et al., 2018 (4).
Case report
Case Operation Procedure
Case 1: A P1A0 woman of 28 years old arrived at RSUD Dr. Moewardi to undergo an infertility treatment. Patient is seen with a moderate general condition, composmentis History, the patient has one child aged 5 years Clinical exam: supple abdomen, no tenderness, no vaginal bleed or discharges. The patient was diagnosed with bilateral non-patent tubes, a five years secondary infertility. Laboratory results: creatinine 0.6 mg/dl, blood sodium 134 mmol/l, blood chloride 108 mmol/l, hemoglobin 11.1 g/dl, hematocrit 33 percent, erythrocytes 3.77 million/μl.
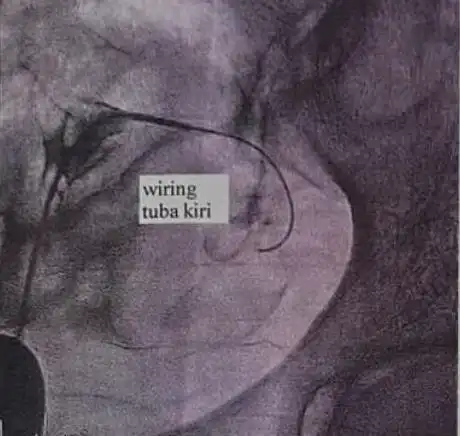
During fallopian tube recanalization, injections of hyoscine butyl bromide (30 mg every 8 hours) and ketorolac tromethamine (12 mg every 12 hours) were given. Prior to the FTR procedure, ECG recordings were performed on the patient and normal blood pressure was obtained. Furthermore, preparation of the vulva was carried out with liquid betadine and alcohol. The patient is positioned in the lithotomy position for insertion of the speculum. The salpingography canula is inserted into the cervix and contrast is given, so that the contrast fills the cervical canal of the uterine cavity. It can be seen that the contrast doesn’t fill the fallopian tubes, the uterus is in anteflexion position. Cervical canal elongation was obtained. The recanalization procedure was performed with a 4Fr vertebral catheter and 0.032 x 150 cm wire to the left fallopian tube, the results showed total occlusion of the left fallopian tube (6.38 mm). The patient complained of pain so she was immediately given an IV injection of 1-gram metamizole sodium monohydrate. The patient complained of nausea, so she was given an IV injection of 4 mg Ondansentron. The second maneuver was performed with a 5Fr vertebral catheter and 0.035 x 150 mm wire to the left fallopian tube. The patient did complain of severe pain by the time the procedure is completed. Then fluoroscopy was performed with Iodixanol contrast 32- 60 cc for a duration of 20.49 minutes at a dose of 61 mGy. The patient was transferred to the ward. The patient was allowed to go home on the same day and scheduled for follow-up in 3 months later. When the patient was allowed to go home, the vital signs were normal.
Case-2: A 29-year-old P0A0 woman who had been infertile for two and a half years arrived at RSUD Dr. Moewardi to undergo an infertility treatment program. The patient came in a good general condition, compos- mentis, and vital signs within normal limits. The patient was diagnosed with primary infertility and had a history of anxiety problems. Furthermore, HSG will be repeated on the patient and she is given 1×2 Clomiphene citrate therapy. A few days later, the patient was diagnosed with non-patent tubal infertility The results of awareness assessment E4M6V5, blood pressure 120/80 mmHg, pulse 86x/minute, temperature 36.4oC, and respiratory rate 20x/minute regularly. Laboratory examination of the patient showed blood sodium 137 mmol/l, blood potassium 4.2 mmol/l, blood chloride 100 mmol/l, non-reactive HBsAg, hemoglobin 14.1 g/dl, hematocrit 42 %, leukocytes 9.500 /μl, platelets 267.000 /μl, erythrocytes 4.80 million/μl, blood-type B with positive rhesus, PT 12.7 second, APTT 27.0 second, INR 0.930, blood glucose 106 mg/dl, total protein 7.0 g/dl, albumin 4.5 g/dl, globulin 2.5 g/dl, creatinine 0.6 mg/dl, urea 17 mg/dl, and abnormal results were obtained on SGOT 35 μ/l and SGPT 35 μ/l.
Seven months prior, the patient underwent an HSG in a private hospital and clinical exam did reveal a flat external uterine orifice, an erosion, a vaginal discharge. HSG was performed, 3 times: 5 cc, 4 cc, and 4 cc. With the patient in antero-posterior position photos were taken, right oblique, left oblique with as a result: normal uterine size and shape, both tubes are not visualized, no spillage is seen from both tubes, no hydrosalpinx, normal uterine impression, both tubes non-patent.
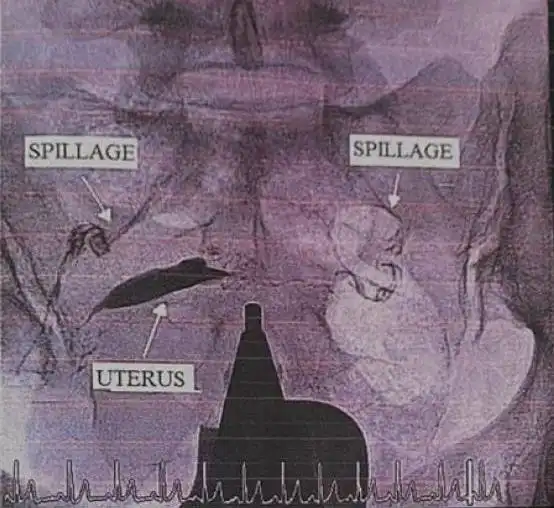
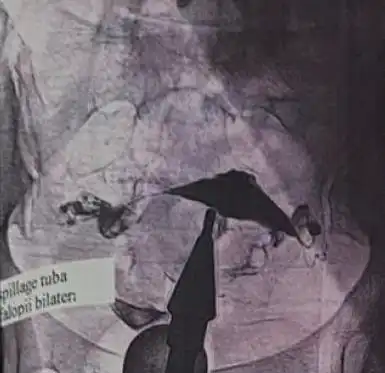
It was decided to perform a hysterosalpingography. Prior to the FTR procedure, an ECG record was performed on the patient and a blood pressure of 167/91 mmHg and a pulse of 100 x/minute were obtained. The usual preparation of the site as above mentioned were performed. Hysterosalpingography was performed using a metal salpingography cannula, contrast medium was injected, it was seen that the lumen of both fallopian tubes were filled with contrast and spillage was observed figure 1. After this first procedure, the patient underwent a fluoroscopy with Iomeprol 400 mg 15 cc contrast for 36 minutes with a dose of 61 mGy and fluoro dose area product 13505 mGycm2.
Case 3: A 28-year-old woman came to RSUD Dr. Moewardi by referral from a private hospital with a diagnosis of bilateral non-patent fallopian tubes. The patient came in with a good general condition, compos mentis, and vital signs within normal limits. The patient underwent a chest X-ray and it was found that the size and shape of the hearth were normal, there were no infiltrates nor nodules in both the pulmonary fields, normal broncho vascular markings, sharp right and left costophrenic sinuses, normal right and left hemidiaphragms, trachea in the middle, good bone system, in conclusion both heart and lungs do not show abnormalities.
The patient’s laboratory examination showed hemoglobin 12.2 g/dl, hematocrit 37 %, leukocytes 5.7000 /μl, platelets 311.000 /μl, erythrocytes 4.67 million/μl, blood-type A rhesus positive, albumin 4.9 g/dl, creatinine 0.7 mg/dl, urea 21 mg/dl, blood potassium 4.5 mmol/l, non-reactive HBsAg, non-reactive anti-HIV-I. Abnormal results were found for total protein 5.9 g/l, blood sodium 130 mmol/l, and blood chloride 107 mmol/l.
A few weeks earlier, the patient underwent an HSG examination and the results showed the bony structure to be normal, no soft tissue mass nor swelling was seen, +/- 10 cc of water soluble contrast was inserted into the uterus through a catheter attached to the OUE, the contrast appeared to fill cavum uteri cervical canal, no contrast is seen filling the right nor the left fallopian tube, the cervical canal appeared normal, regular mucosa, uterus in anteflexion, size of uterine cavity looks normal, no spillage right and left, so that the conclusion leads to a bilateral cornual spasm.
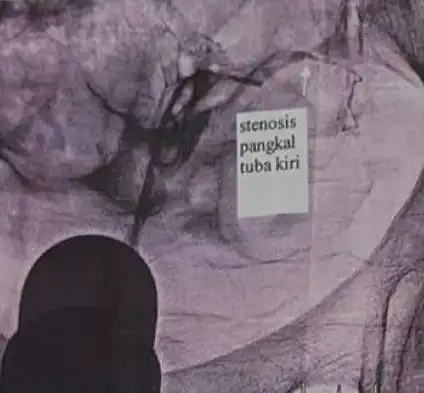
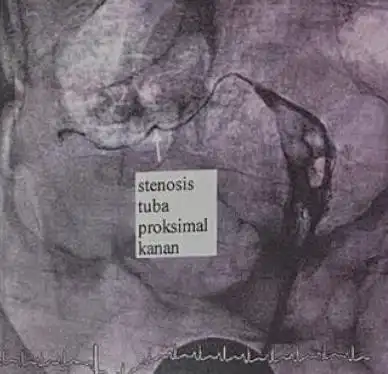
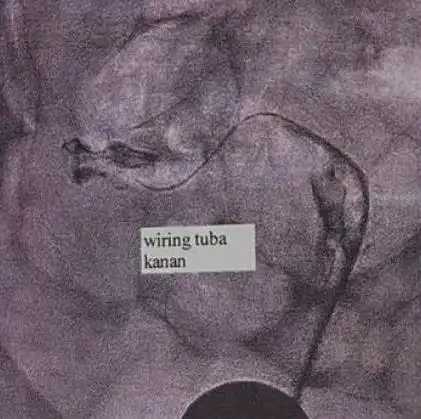
The decision was made to perform surgery in the form of a recanalization procedure of the fallopian tubes. Prior to the FTR procedure, a normal ECG was recorded and a blood pressure of 135/85 mmHg with a pulse 86 x/minute were obtained. Hysterosalpingography was performed resulting in bilateral patent tuba, a stenosis was seen at the base of the left tube figure 2 b and c and proximal to the right tube (c), contrast was injected into the right tuba. Insertion of the 4 Fr Vertebral Diagnostic Catheter is performed, followed by hysterosalpingography (figure 2. d -e) (d). Insertion of the 0.032-inch Guidewire through the 4 Fr Vertebral Diagnostic Catheter, followed by hysterosalpingography (e). The procedure is completed, the 4 Fr Vertebral Diagnostic Catheter and the wire are removed. Fluid intake: 100 cc, output bleeding: 10 cc, urine: 200 cc. Then a fluoroscopy was performed on the patient with Iomeprol 400: 60 cc contrast in 6 minutes 58 seconds with a dose of 210 mGy and fluoro dose area product 21608 mGycm2. Resulting in bilateral patent tubes figure 3.
The fallopian tube, as a place of fertilization in the reproductive process, is very dependent on the healthy condition of its anatomy and physiological function. Disturbances in the anatomy and function of the fallopian tubes can create pathological conditions in women, including infertility, infection, and ectopic pregnancy Su et al., 2022 (5). In studies on infertility in women, tubal factor infertility is the most common cause of infertility. So that the diagnosis and assessment of tubal abnormalities can help couples who are going through a pregnancy program to find out the causes of infertility and treat them Dun & Nezhat, 2012 (6)). In a study from the UK, several causes of tubal factor infertility included chlamydia infection, PID, to salpingitis Price MJ et al., 2016 (7).
Diagnosis and examination of the fallopian tubes can be done through Hysterosalpingography, Hystero- salpingo-contrast sonography, and gynecological endoscopy. This examination can assess tubal patency or tubal compliance without obstruction which supports the function of the fallopian tubes in pregnancy. HSG has a higher sensitivity (65%) and specificity (83%) in assessing tubal patency than gynecological endoscopy. A faster diagnosis and less exposure to radiation can be done with hystero-salpingo-contrast sonography (6) Tubal obstruction can inhibit fertilization and the passage of embryos so that treatment is needed to restore the patient’s reproductive function.
One of the methods to treat non-patency in the tube is Fallopian-Tube Recanalization (FTR). In various studies, currently recanalization of the fallopian tubes increases with 50% the chance of conception in individuals after tubectomy and with 68% in salpingitis patients Mohan et al., 2018 (4). This figure has increased a lot since the FTR was first introduced in the 19th century. Tanaka et al. 2011 (8) described the development of FTR since the surgical approach for the treatment of proximal obstruction was conceived. In the 19th century, FTR was developed into falloposcopy for the treatment of cornual obstruction and endoscopic catheterization. Kohi et al, 2021 (9)) stated in his study, that currently, FTR is a minimally invasive procedure with a hysterosalpingogram for evaluation. A. Tanaka et al., 2017 (10) in a recent study reported that the tubal recanalization method with a combination of hysteroscopy and laparoscopy was successful in increasing pregnancy to birth. Another study described other methods of implementing FTR, namely FTR with radiological interventions that can be carried out more minimally invasive (Mohan et al., 2018 (4). The main point is, Fallopian Tube Recanalization begins with diagnostic steps such as HSG or Salpingography in the lithotomy position. This procedure is performed to assess tubal patency and the location of the tubal obstruction. HSG is performed with the addition of contrast through the cervix as to assess the proximal obstruction of the fallopian tube. The recanalization maneuver is performed with a 5-French or 3-French catheter. If there has been spillage of contrast in the peritoneal cavity, the tubal obstruction has been resolved (4,9). Anesthesia is required during the procedure to minimize pain and discomfort for the patient. In the cases discussed, fluoroscopy was still performed to ensure the success of FTR. This method can maximize the success of FTR and minimize the risk of complications from the FTR procedure.
Kohi described the outcomes of FTR, including 84% of pregnancies occurring 1 year after FTR and 41% of them through full-term births (9) . A woman’s chance of getting pregnant after the FTR procedure is 27%, with another 4% having an ectopic pregnancy. In the cases that have been described, the outcome of the FTR procedure was indicated as successful after visible contrast spillage in the peritoneal cavity. In one of the cases, the pregnancy occurred spontaneously after 8 weeks, and the other two cases did not result in pregnancy.
Conclusion
The fallopian tube as a place of fertilization has a very big role in the reproductive process. Disturbance of the fallopian tubes can cause several pathological conditions in women. One of them, namely tubal obstruction that can inhibit fertilization and the passage of conception results from fertilization on the uterine wall, so that treatment is needed to restore the patient’s reproductive function. One of the methods to treat non-patency in the tube is Fallopian-Tube Recanalization (FTR). FTR can increase the chances of women who were previously infertile to be able to experience pregnancy.