Authors / metadata
DOI: 10.36205/trocar2.2023002
Abstract
Introduction: Since described by Harry Reich in 1989, laparoscopic hysterectomy is increasingly practiced worldwide with little data in African publications.
Objective: we aim to review the epidemiological, clinical, and therapeutic aspects of patients who underwent first laparoscopic hysterectomy in a tertiary hospital in Yaoundé, Cameroon.
Materials and Methods: A descriptive cross-sectional study with retrospective data collection over a period of 3.5 years from January 1, 2019, to July 31, 2022, has been conducted It included 32 patients who underwent laparoscopic hysterectomy for benign disease from the Gynecological Surgery Department of Yaoundé Gyneco-Obstetric and Pediatric Hospital (YGOPH). Gynecological malignancies managed by laparoscopy have been excluded. Data were collected from the surgical registers and patients’ files and analyzed with SPSS 26.0 software. A P value less than 0.05 was considered statistically significant.
Results: The frequency of laparoscopic hysterectomies compared to all cases of hysterectomies was 15.71% (44/280); among them 32 laparoscopic hysterectomies for benign disease (11.42%). The frequency of abdominal hysterectomy was 81.78% (229 cases) and vaginal hysterectomy was 2.5% (7 cases). The patient’s median age was 49 (34-67) years. 96.87% of patients (31 cases) were above 40 years of age (y/a) and 59.37% (19 cases) were pauciparous. 46.87% (15 cases) of them were postmenopausal. 25% (8 cases) of patients had a history of abdominal surgery, 50% of which were a cesarean section. Half of our patients had a BMI ≥30kg/m². The size of the uterus varied from 6 weeks to 15 weeks and was less than 8 weeks in 20 cases (62.5%). Cervical dysplasia was the main indication for surgery in 16 cases (50%), followed by symptomatic myomas in 12 (37,5%). The average operative time was 98.72 ± 49.42 minutes (55min – 240min), the average blood loss was 173±99cc and the postoperative length of stay was 2.80 ± 1.38 days. There was no conversion to laparotomy but two patients presented urogenital fistulas secondary to ureteral lesions which were successfully treated by the urologists.
Conclusion: At the YGOPH laparoscopic hysterectomy for benign gynecological pathologies represented 15.71% of all hysterectomies. Approximately 60% of patients are at least 40 years of age. The two main indications for surgery were respectively cervical dysplasia and symptomatic myomas. Complications are rare but are severe.
Introduction
In Women, after cesarean section, hysterectomy is the most performed surgery in the world (1–3). It is defined as the surgical removal of the uterus. In 90% of cases, it is performed for benign indications, including uterine fibroids, abnormal uterine bleeding, endometriosis, and precancerous lesions of the cervix (4). Several approaches are known today, including the vaginal and laparoscopic routes which are considered to be minimally invasive procedures. The latter are increasingly used in developed countries. Indeed, several learned societies currently recommend the vaginal route in the management of benign pathologies and in the event of a relative or absolute contraindication to the latter, they recommend the laparoscopic route (5). Since the choice of approach is not standardized, these societies have developed decision-making algorithms to help practitioners. These take into consideration the size of the uterus, the vaginal access, and the type of pathology. Also, factors such as physician preferences (training, experience) and availability of resources (facility, equipment, support) are important for decision-making (6). In Finland, 32% of hysterectomies are now performed laparoscopically (7). Similarly, a study carried out in the United Kingdom in 2017 showed that the percentage of hysterectomies performed by laparoscopy had increased from 20.2% in 2011 to 47.2% in 2017 (8). In Africa, the laparoscopic route is still poorly practiced (3.92%) (9–11). Indeed, it was in the 2000s that Cameroon embarked on the practice of laparoscopic hysterectomies (12). At Yaoundé Gyneco-Obstetrics and Pediatric Hospital (YGOPH), the first laparoscopic hysterectomy was performed in 2019. Given the advent of this method in our environment, the current study was conducted with the aim of knowing what were the epidemiological and clinical profiles of patients undergoing laparoscopic hysterectomy for benign gynecological pathology.
Material method
This is a descriptive cross-sectional study with retrospective data collection over a period of 3.5 years from January 1, 2019, to July 31, 2022, in the gynecology department of YGOPH. It included patients of any age, with a benign gynecological pathology in whom a total hysterectomy by laparoscopy had been performed and whose medical file was complete. It excluded patients who had undergone a subtotal hysterectomy and those whose anatomopathological examination of the surgical specimen returned with the diagnosis of cancer.
For each file, the socio-demographic, clinical, and paraclinical data of the patients have been collected. The primary endpoints were age, parity, menopausal status, history of abdominal surgery, and surgical indication. The size of the uterus was estimated on ultrasound in centimeters. The secondary endpoints were the duration of the operation, the volume of intraoperative blood loss, the postoperative length of stay, the intraoperative complications, and complications during the first 3 postoperative months. Pre and perioperative characteristics have also been recorded. Operative time was defined as the period from incision to complete closure, excluding room and anesthesia time. Blood loss was estimated by suction container contents with irrigation fluid subtracted.
Data were recorded and analyzed with SPSS 26.0 software. Means (+- SD), frequencies (%), and ranges were used to describe population characteristics and outcomes. A p<0.05 value was considered statistically significant. The research ethics committee of Yaoundé Gyneco-Obstetric and Pediatric Hospital (YGOPH) approved the study protocol (No. 317/CIERSH/DM/2022).
Results
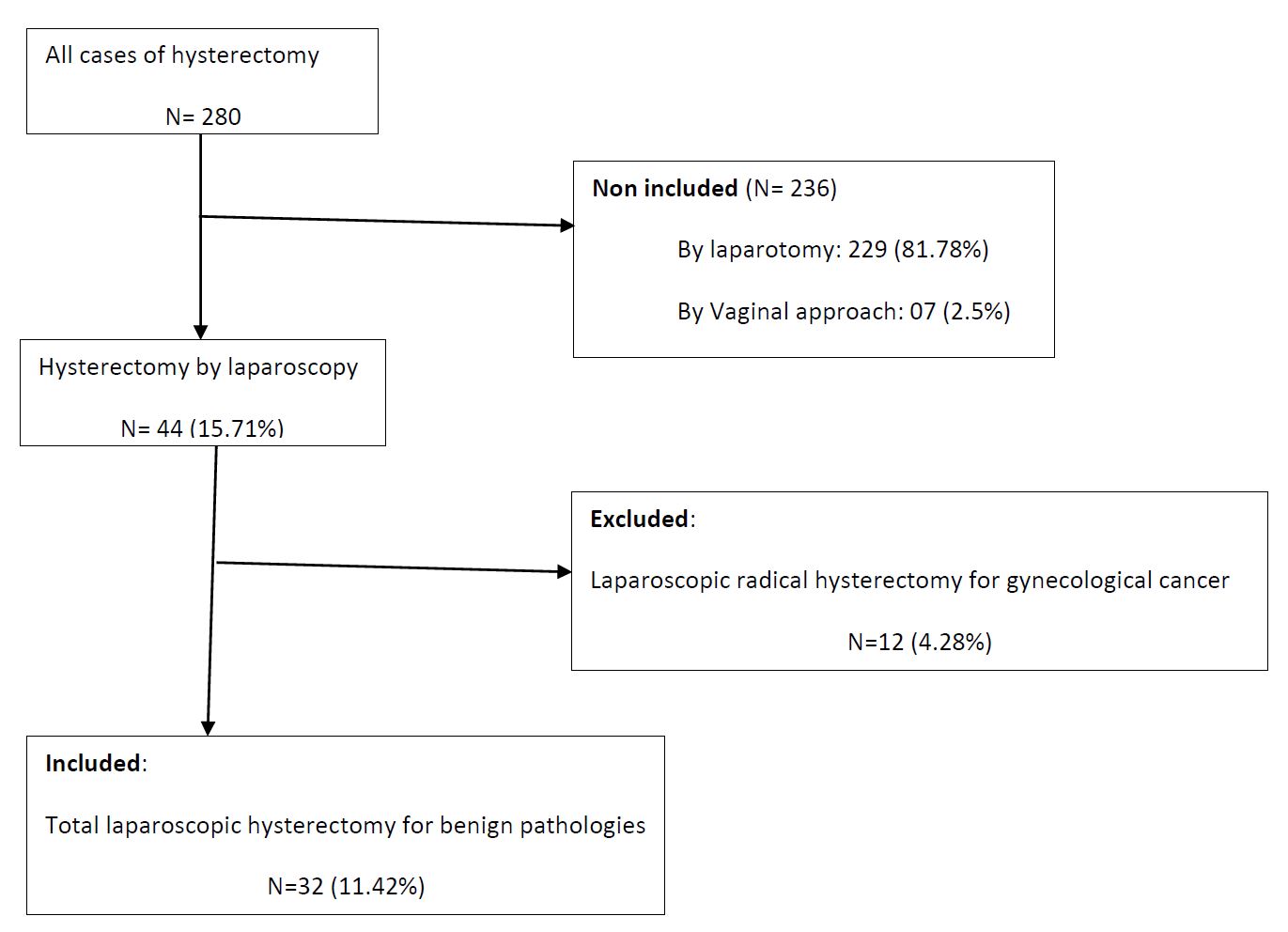
During the study period, 280 hysterectomies have been recorded, of which 44 were performed by laparoscopy with 32 cases for benign pathologies, giving a frequency of 15,71% (Figure 1).
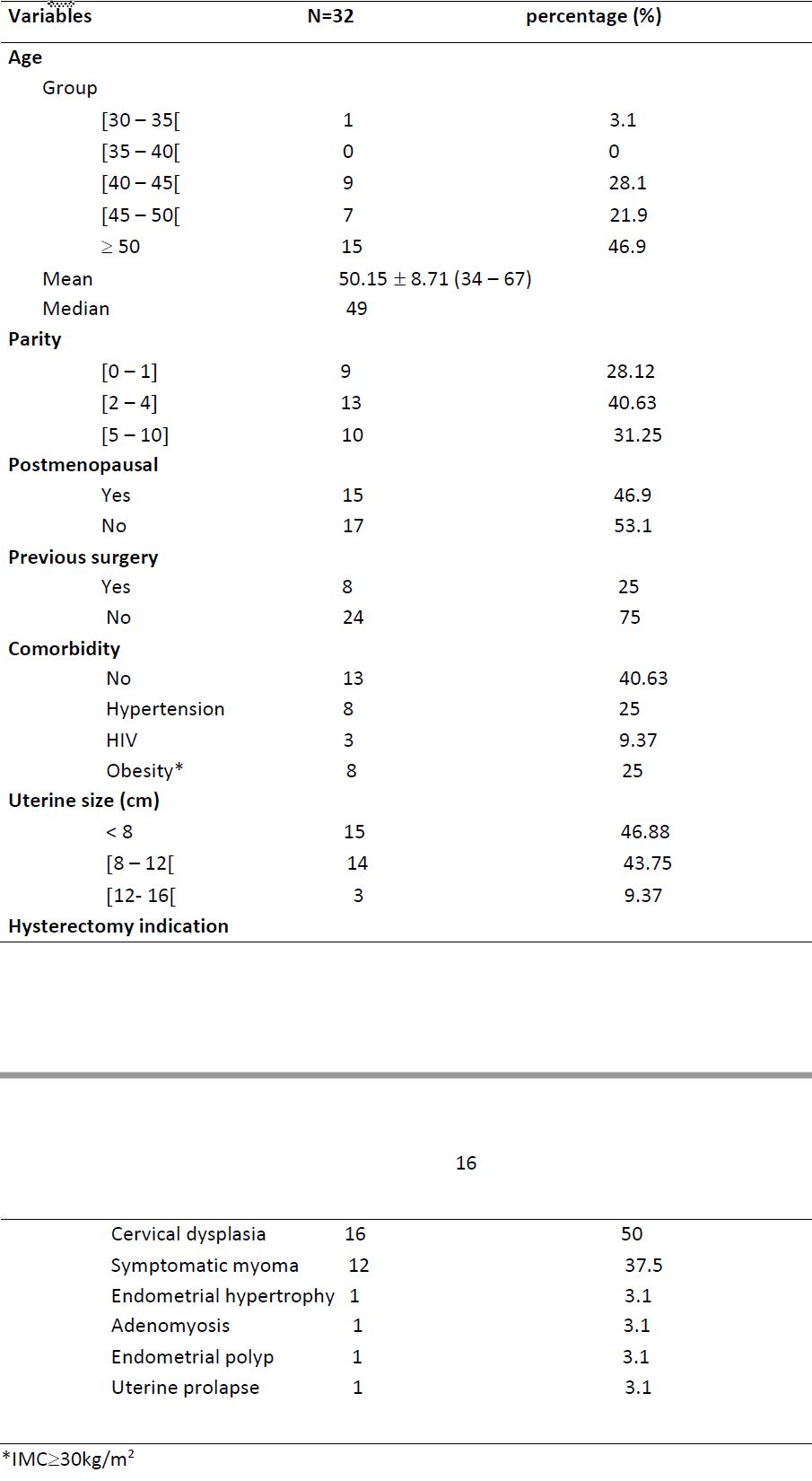
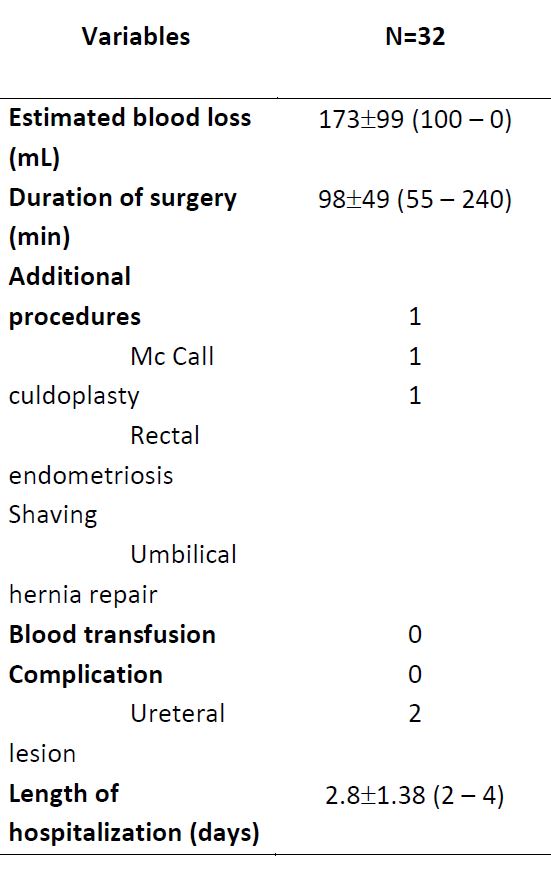
The pre operative and peri operative characteristics of the women who underwent total laparoscopic hysterectomy (TLH) are presented respectively in Table 1 and Table 2.
The median age of patients was 49 (34-67) years. In 96.87% of cases, patient’s age was at least 40 y/o. 46.9% of them were postmenopausal (Table 1).
25% of operated patients had a history of abdominal surgery and in half of the cases, it was a history of caesarean section. 25% of our patients had a BMI ≥30kg/m². 53.12% of patients had a uterine size greater or equal to 8 cm among which three cases (9.37%) greater or equal to 12 cm.
The main indications for hysterectomy were precancerous lesions (50%) followed by symptomatic myomas (29%) (Table 2). Abnormal uterine Bleeding was the leading symptom representing 46,87% of cases (leiomyomas, endometrial hypertrophy and polyps, adenomyosis).
The mean estimated blood loss and postoperative hospital length of stay were respectively 173±99mL and 2.80±1.38 days. The procedure lasted 98±49 minutes on average.
Two patients were readmitted for watery vaginal discharge, which revealed to be ureteral lesion after dye test. Both lesions were in the right side. Thus, the total rate of complication was 6.25% (2 patients).
The follow-up of the patients during the three months after the operation was unremarkable.
Discussion
With advances in medical technology, equipment, and training, the practice of hysterectomy has been revolutionized by laparoscopy. In our study, 280 hysterectomies were performed, of which 81.78% were abdominal, 15.71% laparoscopically (11.42% for benign disease), and 2.5% by vaginal route. The trend observed in Cameroon (13), South Africa (14), Hong Kong (15), China (16) and India (17) showed that laparoscopy was the third surgical route after the abdominal and vaginal route. According to the Canadian Society of Obstetricians and Gynecologists and other authors, in case of benign conditions, the vaginal route should be recommended and preferred whenever possible followed by laparoscopy because of morbidity associated with the abdominal route including longer recovery time, longer hospital stay, higher per operative blood loss, more pain and postoperative infection (5-18-19-20). Due to the lack of a national hysterectomy registry or a nationwide analysis of hysterectomies, it is difficult to assess the trend in the practice of laparoscopic hysterectomy in Cameroon. But it would seem that since the first cases of hysterectomy published by Belley (12), the practice has been on the rise.
In our study, the mean age of the patient was 50.15 ± 8.71 years, which correlated with other studies: 47 ± 6.7 years; 49.1 ± 9.0 years; 48 ± 9.9 years (12-13-17). This mean age can be explained by the fact that it represents a perimenopausal period, in that age group surgeons generally propose a radical treatment for the management of benign pathology. A younger average age of 34 y/o was found by Shekar in India (21). He did attribute this to the fact that in the cultural environment, women often self-select to get rid of their health problems after they have had the desired number of children, all of whom have survived to a certain age.
In our study, 71.88% of women had at least two children. This result is similar to that of Aboulfotouh et al in Qatar and Sudhev et al in Thailand who also found a majority of pauciparous in their study (22 – 23).
In the current study, the main indication of hysterectomy was severe cervical dysplasia in 50% of cases, followed by symptomatic leiomyoma in 37.5% of cases. The predominance of cervical dysplasia can be explained by the opening of a gynecological oncology service in our hospital and daily cervical cancer screening during the study period. This result is in contrast with most studies that find that leiomyomas are the main indication for laparoscopic hysterectomy (12, 13, 16, 17, 24). In Germany, Stang showed that the treatment of myomas was a hysterectomy in 60% of cases (25). We think that this attitude should only be considered for symptomatic myomas in a woman who no longer wishes to have children and for whom other therapeutic options have failed. In cases of myoma or other pathologies such as adenomyosis, the excess uterine volume represented a limit to the laparoscopic approach. In addition, since the warning statement of the FDA on the use of power morcellation in the case of myomectomy and hysterectomy, patient must be carefully selected (26).
More recently, numerous studies have shown that obesity, previous surgery, and a large uterus are no longer limiting factors for laparoscopic hysterectomy (27, 28, 29). There is no consensus definition of a large uterus. The American College of Obstetricians and Gynecologists (ACOG) considers 280g or 12 Weeks as a cut-off value for definition (30). Our study found a history of a cesarian section in 12.5% of cases, obesity in 25% of cases, and only 3 patients (9,37%) had a uterus size greater than 12 weeks. However, for young gynecologists starting laparoscopic hysterectomy in low-resource income as in our case, all the above limiting factors must be taken into account due to the fact that we are almost lacking adequate resources and sometimes additional procedures have to be carried out; this may extend the duration of the operation and lead to complications.
Total laparoscopic hysterectomy is well known to be safe and effective with a complication rate of 0.52% to 6.2% (31,32, 33, 34, 35). This is in line with the current study, where we found a total rate of complications at 6.25%. In contrast, some studies showed a high complication rate of around 11.1% and the inexperience of surgeons was the main explanation (36). To decrease the complication rate, Garry and Twijnstra suggested that surgeons need to perform 25 cases to complete the learning curve (37). For Terzi, the learning curve can also be measured by the reduction in operating time, even if some factors can affect the difficulty of the surgery, such as a large uterus, previous pelvic surgery, and high body mass index (35). In low-income countries, inadequate or defective surgical equipment can affect the learning curve. The two cases of ureteral injury in the current study did occur respectively in the third and fifth cases of total laparoscopic hysterectomy. Both patients were successfully surgically managed by the urologic surgeons. We did not have any conversion to laparotomy; however, the rate of conversion can reach 6.6% and is most often found at the beginning of the learning phase even if it is not rare to find it after having completed the learning curve (34, 38).
The mean operating time in our study was 98 minutes (55-240 minutes) which correlated with other studies (35, 39). But it may be longer if there is an additional procedure or factors that may affect the difficulty of the surgery. We performed three additional procedures: rectal endometrial shaving, an umbilical hernia repair, and a McCall culdoplasty for uterine prolapse.
The advantages of the laparoscopic approach are less blood loss, lower transfusion rates, better cosmetic results, lower rates of adynamic ileus, faster return of bowel function, and overall faster recovery (40). In the current study, the average length of hospitalization was 2.8±1.38 days (2-4 days) and the average blood loss was estimated at 173 ml (100-250). A recent report also featured the safety and feasibility of outpatient total laparoscopic hysterectomy options for carefully selected patients even in the presence of obesity, leiomyomas, severe adhesions, or endometriosis (41, 42, 43).
The major limitation of our study was the retrospective design.
Conclusion
Total laparoscopic hysterectomy is increasingly being performed in our department representing 15.71% of all hysterectomies. The current study presents our initial experience with 32 cases of benign pathologies. Approximately 60% of patients are at least 40 years old. The two main indications for surgery are respectively cervical dysplasia and symptomatic myomas. All patients underwent total laparoscopic hysterectomy with a complication rate of 6.25%. This study demonstrates that even if it requires a learning curve, laparoscopic hysterectomy is a feasible and safe procedure in low-resource income settings where surgical instruments are frequently inadequate.