Authors / metadata
DOI: 10.36205/trocar2.2023006
Abstract
Assessment of abdominal pain in puerperal women can be challenging given that physiological and often self-limited benign causes predominate in this clinical context, although the etiological spectrum is wide and includes serious and potentially fatal causes. The paper presents a case of left ovarian thrombophlebitis, clinically manifested from the fifth day of puerperium in a 30-year-old patient. Clinicians should have a high degree of suspicion of rare adnexal thromboembolic events in postpartum period when frequent symptoms (fever, pain) and analytical changes (leukocytosis, increased C-reactive protein) occur in association with the imaging findings of edematous ovary with vascular congestion, even if there are other possible explanations for such a clinical situation.
Introduction
Abdominal pain in puerperal women can be caused by common and self-limited causes, while a high degree of caution is required in order not to miss the diagnosis of conditions that occur during this period and can be life-threatening (1). Although it is important to consider that physiological changes occur and may mimic some pathological situations, the patient’s complaints should not be lightly devalued and attributed to physiological changes alone without a detailed evaluation (1, 2).
Thromboembolic complications are more common in puerperal than in other apparently healthy women. Ovarian vein thrombosis (OVT), in particular may easily be overlooked, being infrequent clinical condition. The incidence of septic pelvic thrombophlebitis is estimated to be as low as 1/3000 deliveries (3, 4). This diagnosis should be considered when approaching a puerperal woman with abdominal pain. Although it has been more often reported on the right side, probably due to anatomical reasons, site variations cannot be ignored, as indicated by the even rarer cases of left-sided OVT presented here.
Case report
A 30-year-old G0P0 woman, with an unremarkable medical history and an uneventful pregnancy, had a spontaneous vaginal delivery at the gestational age of 40 weeks and 1 day, from which resulted a healthy male newborn, weighing 3750 g (Apgar score: 9 at the 1st and 10 at the 5th minute). During the first 4 days postpartum, the patient presented a normal evolution, but remained hospitalized to accompany the newborn submitted to phototherapy due to benign neonatal hyperbilirubinemia.
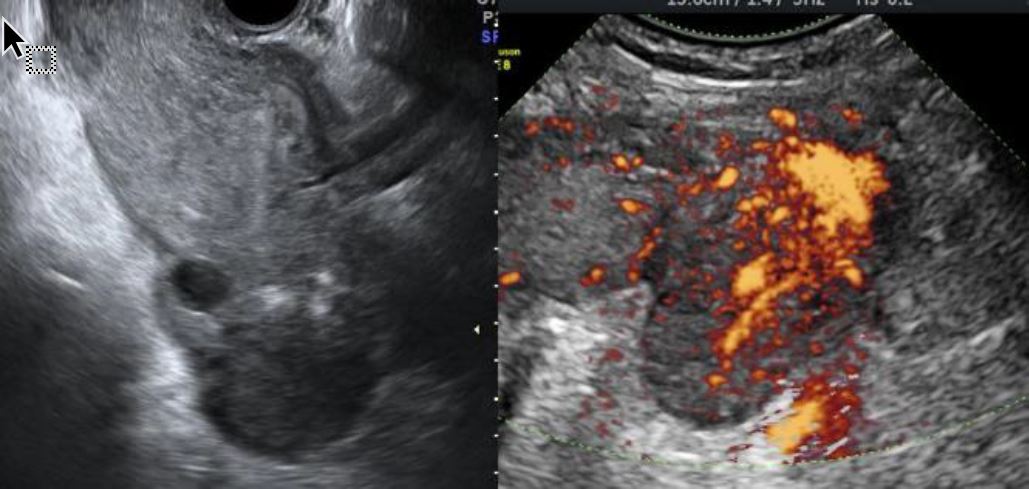
On the 5th postpartum day, she developed fever (maximum tympanic temperature of 39.8°C) and left pelvic pain. No other relevant symptoms or signs were identified. Laboratory assessment showed blood hemoglobin 9.7g/dL, leukocytosis (16,06 x 109/L with 88% neutrophils), elevated C-reactive protein (CRP; 157,5mg/L) and a urinary infection caused by Streptococcus pyogenes (sensitive to penicillin, clindamycin, and trimethoprim-sulfamethoxazole). Ultrasound revealed an endometrial cavity with non-vascularized 14-mm-thick amorphous content, edematous enlarged left ovary, apparently without pathological adnexal formations, and congested ovarian branches originating from left internal iliac artery (Figure 1). The mobilization of the left adnexa by ultrasound probe was very painful. There were no other relevant findings. Angio-CT visualized a vascular pathological process, interpreted as most likely a left ovarian vein thrombophlebitis with a partially permeable lumen (Figure 2). A diffuse densification and very little fluid involving the left ovarian vein (which had a reduced lumen caliber), in association with a small amount of free fluid on the left parieto-colic gutter were observed. The left ovary was large and some reactive para-aortic and primitive iliac lymph nodes were identified (Figure 2).
The presumptive diagnosis of septic thrombophlebitis was accepted. The patient was medicated with low molecular weight heparin (LMWH; 60mg of enoxaparin every 12 hours) and intravenous antibiotics (ceftriaxone 1g once daily and metronidazole 500mg every eight hours). After 6 days, she was subjectively better while the fever had subsided. Blood cultures were negative. Antibiotics were suspended but LMWH was maintained. On the following day the patient was discharged, medicated with LMWH and acetylsalicylic acid 150mg/daily orally.
Additional ethological studies included searching for antiphospholipid syndrome, prothrombin and Leiden V factor anomalies, all of which were negative. From the autoimmune panel the only positive results were antinuclear antibodies (ANA) 1:160 and anti-extractable nuclear antigen (ENA) antibodies displaying a dense fine speckled pattern (DSF) 70.
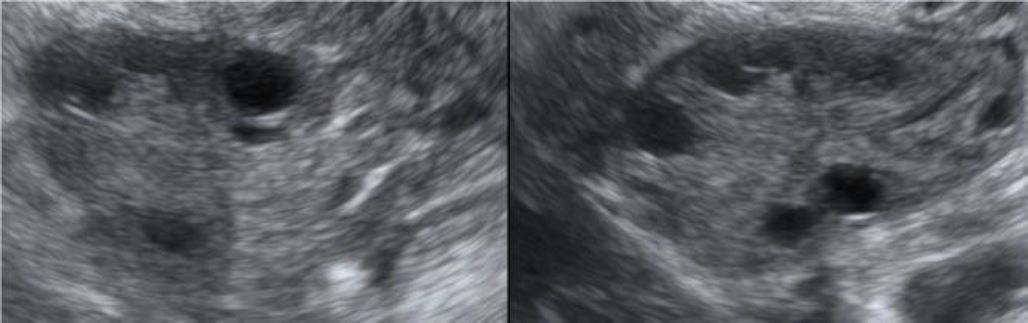
The patient was counseled to stop the LMWH, but to keep taking acetylsalicylic acid and to maintain an active lifestyle. The patient´s further evolution was favorable. Both ultrasound (Figure 3) and CT scans, performed 3 months later, demonstrated a complete resolution of the left ovarian vein thrombosis. She intended to move to another country, being advised to seek a medical appointment in the country she was moving to, in order to continue the etiological investigation and the follow-up.
Discussion
Postpartum OVT is uncommon, occurring in 0.05% to 1.8% of vaginal deliveries and in 1 to 2% of cesarean sections (5, 6).Puerperal patients are physiologically in a prothrombotic state and so, their risk of thrombosis is significantly higher when compared to a non-pregnant patient. The relative risk for venous thromboembolism was 4,29 higher during pregnancy and postpartum in a 30-year population-based study conducted in the USA (7). Other populational study conducted in the United Kingdom estimates that the risk of venous thromboembolism (VTE) is increased by 22-fold in the postpartum period (8).
The increased levels of estrogen, coagulation factors, von Willebrand factor and platelet activating factors contribute to hypercoagulability. There is also greater chance of endothelial damage. If there is bacterial contamination of the ovarian vein in the course of the delivery, a variant of OVT (i.e. septic thrombophlebitis) may arise, which can in turn make the OVT diagnosis even more challenging (9). Some risk factors have been postulated, such as maternal age higher than 35 years and black ethnicity; in these women, the risk is estimated to be increased by 38% and 64%, respectively (10). Other risk factors have been associated with thromboembolism, such as thrombophilia [the factor with the highest odds ratio, according to a national study conducted in the USA, OR 51.8 (38.7-69.2)], erythematosus lupus, heart disease, sickle cell disease, obesity, fluid and electrolyte imbalance, postpartum infection, and transfusion (10). Of these, only the urinary infection, could be considered in our patient. Apart from the hypercoagulable state, inherent to any pregnant or puerperal woman, other risk factors for OVT are multiparity and surgery, which were not present in this case.
OVT, a potentially life-threatening consequences, is a difficult diagnosis to make since its symptoms tend to be non-specific and mimic many common conditions. It occurs predominantly on the right side, presumably due to anatomical factors (uterine dextrarotation during pregnancy and inferior vena cava compression) (5, 9). Thus, often presenting symptom is the right-sided low abdominal pain, isolated or accompanied by other complaints. Systemic symptoms may also be present, such as fever, nausea and vomiting (5, 9, 11-13). Our patient presented abdominal pain on the left side, fever and chills 5 days after the delivery. Literature indicates that the OVT symptoms usually arise within the first 7 day postpartum, however, their onset can happen during 4 postpartum weeks (9, 13). Regarding the main presenting symptom, the abdominal pain, causes of acute abdomen should be excluded, namely appendicitis, endometritis, ovarian torsion and tubo-ovarian abscess. Since our patient was also experiencing fever and chills, infection in the postpartum context was investigated (9).
Even though OVT arises mainly on the right side, the events on the left vein have been described and this possibility cannot be overlooked in patients with left-side symptoms and signs (14, 15). Since the clinical presentation is nonspecific, the diagnosis of ovarian vein thrombosis relies heavily on imaging studies [combined gray-scale and power or color Doppler study, computed tomography (CT) or magnetic resonance imaging MRI)]; there is no consensus regarding the gold standard exam to be offered to the patients with suspected OTV (16).
After assuming the diagnosis of septic OVT (based on the fever, abdominal/pelvic pain, analytical signs of infection, in addition to the patient imaging presentation), therapy should be initiated. There are no guidelines regarding the optimal course of treatment for (septic) OVT. However, in the presence of a venous thromboembolic event, the mainstay of the treatment is anticoagulation for 3 to 6 months until the thrombus resolution, and broad-spectrum antibiotics for the septic cases (5, 9, 11-13, 17). LMWH and antibiotic therapy were prescribed to our patient with excellent clinical and analytical outcomes.
Importantly, since OVT may not be immediately suggested by imaging studies, if a symptomatic patient (in similar clinical situations) does not improve after instituted antibiotic therapy, clinicians should consider adding anticoagulant therapy, after excluding active hemorrhage. This might lead to the progressive resolution of the symptoms, allowing an a posteriori diagnosis of deep vein thrombosis. With modern treatment strategies, mortality has dropped significantly from nearly 50% at the beginning of the 20th century to just over 4% at the end of the 1980s (18, 19).
Conclusion
To summarize, the rarity of adnexal thromboembolic events in the postpartum period requires clinicians to be aware of this complication, because only with a high degree of suspicion it is possible to make a correct and timely diagnosis. Clinical presentation is non-specific, including fever, low abdominal/pelvic pain and analytical changes that can occur in the setting of a normal postpartum (especially after a cesarean section) or with more common, benign and frequently self-limited pathologies. The association of these signs and symptoms, analytical changes and imaging findings of edematous ovary with vascular congestion indicate that the diagnosis of OVT should be considered, confirmed or ruled out, and even treated empirically until it is ruled out, due to the high mortality rate in patients who are not adequately treated in time.
References
Figure 1. Sonographic gray-scale and power Doppler findings in patient with ovarian vein thrombosis. Gray-scale image of the left edematous ovary (left). Vascular engorgement (passive hyperemia) within left ovarian parenchyma visualized by power Doppler (right).
Figure 2. Computed tomography angiography scan of the pelvic region affected by left ovarian vein thrombosis. Axial section showing an enlarged left ovary, with prominent ipsilateral blood vessels (arrow); uterus (1); left ovary (2); right ovary (3).
Figure 3. Ultrasound images of the left ovary (left) and right ovary (right), taken 4 months after ovarian vein thrombosis and showing normalization of the ovarian size and morphology.