Authors / metadata
DOI: 10.36205/trocar2.2023003
Abstract
Introduction: Interstitial ectopic pregnancy is a rare form of ectopic pregnancy, representing 2 to 4% of ectopic pregnancies. It occurs when the embryo implants in the intramural portion of the fallopian tube. There are no current guidelines to decide between medical or surgical approach. Due to the high vascularity of the interstitial portion and thus the risk of cataclysmic hemorrhage, it is recommended to surgeons with little experience in laparoscopic surgery to perform laparotomy, although there is a debate on which route to choose between laparoscopy and laparotomy.
Objective: we present five cases of interstitial pregnancies, successfully managed by laparoscopic cornual resection with good control of hemostasis achieved by intracorporeal encircling suture around the cornual mass.
Cases presentation: Four cases of interstitial pregnancies were successfully managed by laparoscopy. None of ultrasonographic features was clearly in favor of interstitial pregnancy. Gestational ages were between 7 and 11 weeks. The average duration of surgery was 55 minutes. Cornual resection was performed in all cases after intracorporeal purse-string suture around the cornual mass acting like a tourniquet. Blood loss related to the procedure was on average 125 ml.
Conclusion: Interstitial pregnancy is a challenge for clinicians to make accurate diagnosis and adequate treatment. Laparoscopic approach with purse-string suture technique to control bleeding is suitable alternative to laparotomy and is ideal for surgeons skilled with principles of laparoscopic surgery and suturing.
Introduction
The implantation of embryo outside the normal endometrial cavity is described as ectopic pregnancy. When this occurs in the intramural portion of the fallopian tube, it is called interstitial pregnancy; this condition accounts for 2 to 4% of ectopic pregnancies (1,2). However, the exact incidence of interstitial pregnancy is difficult to assess due to its rarity and varying definitions used in the literature.
The term cornual pregnancy is often used interchangeably with interstitial pregnancy by some clinicians (3). However, the term cornual pregnancy should be reserved for pregnancy occurring in a congenitally abnormal uterus. The list of such malformations includes rudimentary uterine horn, bicornuate uterus, unicornuate uterus, the cornual region of a septate uterus or a uterus didelphys (2,4). Interstitial pregnancy sometimes is mistakenly referred to as angular pregnancy which is pregnancy where the embryo implants in one of the lateral angles of the uterine cavity, medial to the utero-tubal junction but outside the fallopian tube.
Interstitial ectopic pregnancy is a high-risk situation which can be life threatening. In fact, because of a large vascular network in this region, in the event of rupture the bleeding can be cataclysmic. The diagnosis must therefore be early done for an adequate management. Traditionally, laparoscopy was the gold standard for the diagnosis of ectopic pregnancy (5). However, currently, the widespread availability of transvaginal ultrasound and rapid assays for serum β-hCG has largely made the use of laparoscopy for diagnostic purposes an obsolete practice. There are no current guidelines to decide between medical or surgical approach. But when it is decided to do the surgery, laparoscopic approach seems to be ideal for surgeons skilled in laparoscopic knotting techniques.We present the Yaounde Gynaeco-Obstetric and Pediatric Hospital’s experience in laparoscopic management of four cases below.
Material method
Four patients were diagnosed with ectopic pregnancy and underwent laparoscopic surgery for their management. All of the operations were performed by experienced surgeon under general anesthesia with endotracheal intubation, in lithotomy position with continuous vital signs monitoring.
In all cases, direct entry with trocar was performed and the abdomen was inflated with CO2. To control the hemostasis, we performed systematically intracorporeal purse-string suture around the cornual mass with Vicryl 1 before the dissection. For cornual resection, blunt and sharp dissection of the cornua was performed with either a monopolar hook or scissors. In some case, we used bipolar energy to reinforce hemostasis. After cornual resection, the uterus was sutured with 2 to 4 simple stitches depending on the length. The operative part was introduced into an endobag, then divided into it by scissor before being extracted through a 12 mm trocar. Blood was extracted into an external reservoir to allow its quantification.
Results
Case 1
A 30-year-old patient with one previous pregnancy ended by miscarriage and past history of pelvic inflammatory disease and chronic use of morning after pill, was admitted to the emergency unit with acute lower abdominal pain without any other associated symptoms in a context of seven weeks of amenorrhea. She presented with blood pressure of 118/84 mmHg and good general state. Abdominal and pelvic examination did not revealed signs of peritoneal irritation. At vaginal examination, there was mild cervical tenderness. Emergency ultrasound revealed right adnexal mass, an empty uterus and no fluid collection in the pouch of Douglas. Laboratory test showed serum β-hCG level of 17 832.71 mUI/ml.
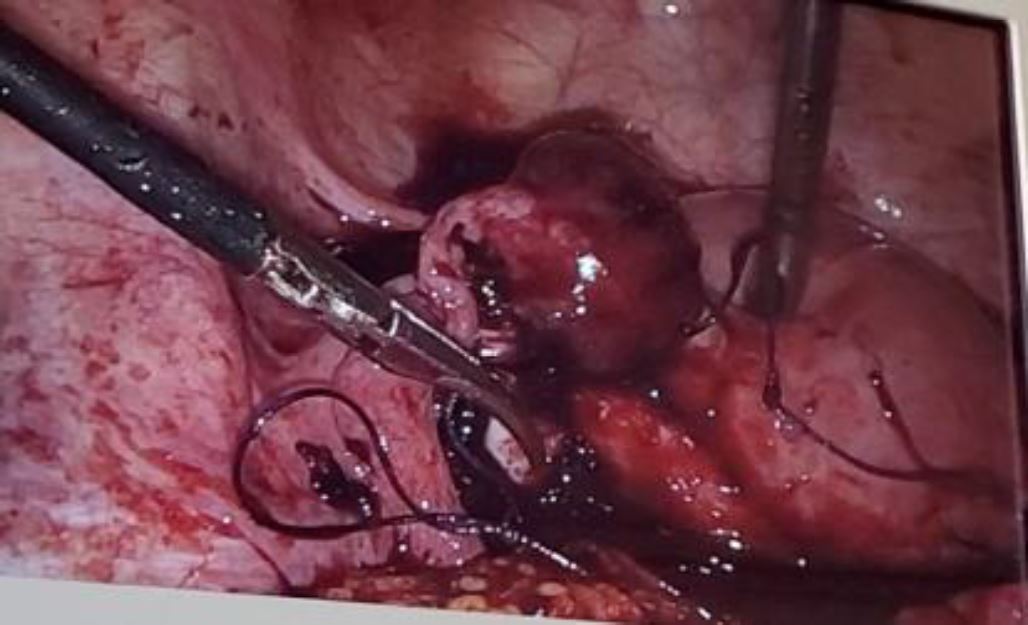
We suspected an unruptured ectopic pregnancy and the patient underwent an emergency laparoscopic surgery, showing an unruptured right interstitial pregnancy of 4cm (Figure 1).
We performed a right cornual resection according to the operating procedures described above. The blood loss associated with cornual resection was estimated at 50 ml. The duration of the intervention was 55 minutes. the patient was discharged after 24 hours of hospitalization. the postoperative period was unremarkable. She had a twin pregnancy 7 months after the surgery and gave birth by cesarean section at 37 weeks.
Case 2
A 20-year-old patient, who was experiencing her first pregnancy, was referred to the emergency obstetric department with acute pelvic pain in the past 24 hours, at 10 weeks of gestation without any other associated symptoms. Her past history was unremarkable.
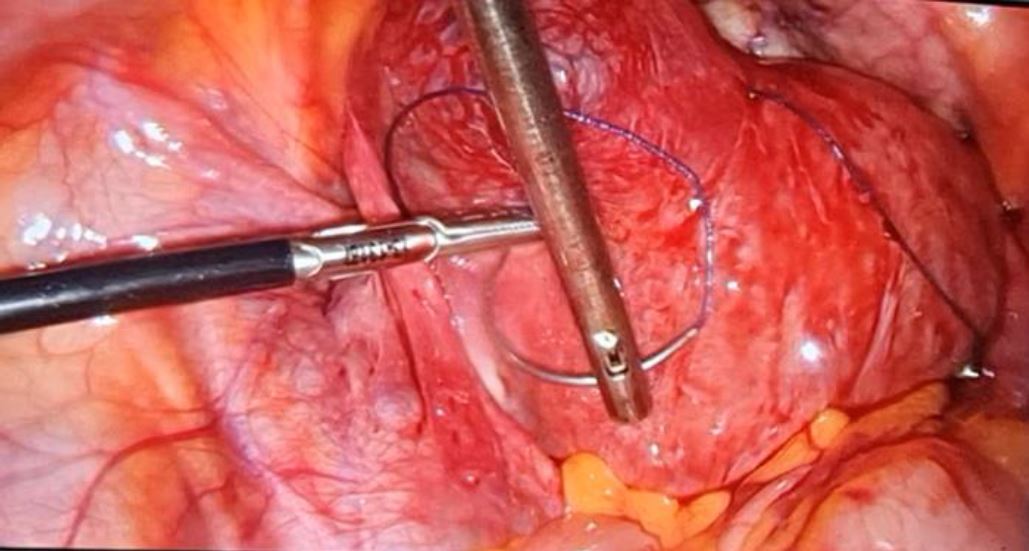
Her assessment on arrival showed blood pressure of 90/50 mmHg, pulse of 140 ppm and mild pallor; abdominal and pelvic examination revealed guarding and tenderness while vaginal examination showed cervical tenderness with fullness in posterior fornix. Culdocenthesis brought back non-clotting blood. Because the patient conditions were worsening, ultrasound was not performed and we did not wait for the results of laboratory before entering the operation room. The resuscitation measures (Crystalloids, plasma expanders and blood transfusion) were immediately initiated by the anesthetists to stabilize the patient and this allowed us to perform an emergency laparoscopy. We found 2000 ml of hemoperitoneum and after aspirating it with a 10 mm canula, we discovered an actively bleeding left ruptured interstitial ectopic pregnancy. Cornual resection was perform according to the operating procedures described above (Figure 2).
The blood loss associated with cornual resection was estimated at 100 ml. The duration of the intervention was 92 minutes. The patient was discharged after 72 hours of hospitalization with hemoglobin level of 9.8 g/dl after she received 1500 ml of blood. She could not follow serum β-hCG level due to financial problems. The postoperative period was unremarkable.
Case 3
A 32-year-old patient, gravida 4, para 3 with three normal vaginal deliveries and past history of regular morning-after pill use, was admitted in the emergency unit for acute lower abdominal pain and vaginal bleeding in the past 24 hours. She presented 10 weeks of amenorrhea with a positive urine pregnancy test.
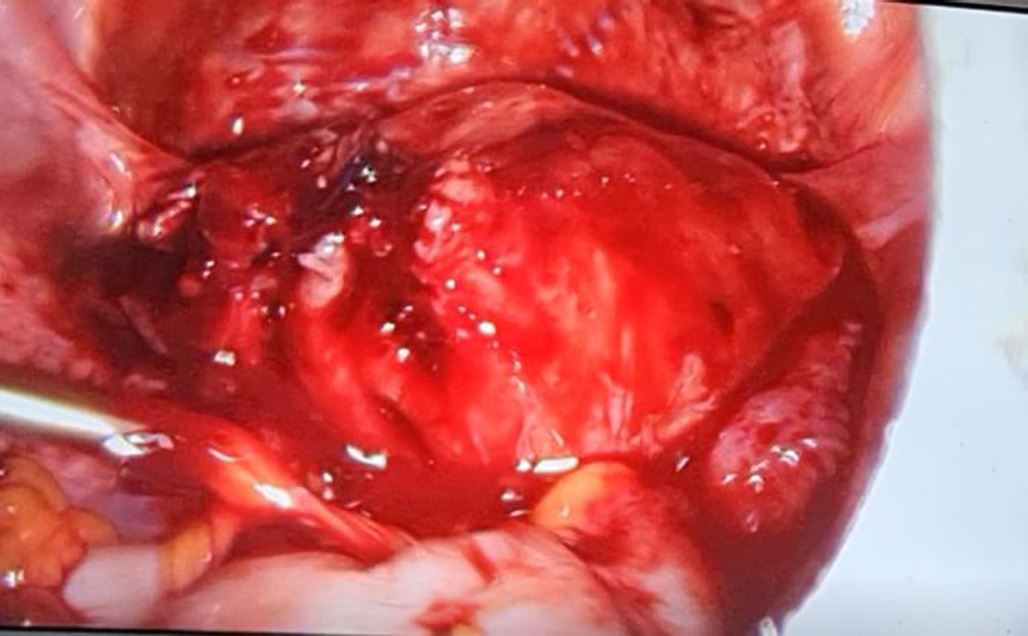
On arrival, the clinical examination was unremarkable apart from pain when the cervix was mobilized on vaginal examination. Transvaginal ultrasound was immediately performed and revealed a non-pregnant uterus with a left adnexal mass of 43mm suggesting an unruptured ectopic pregnancy of 9 weeks 6 days. Laboratory tests showed a serum β-hCG level at 20 893,87mUI/ml, which confirmed an ectopic pregnancy. The patient underwent emergency laparoscopy with cornual resection (Figure 3 and Figure 4).
The operation lasted 1 hour and the blood loss associated with the cornual resection was evaluated at 250 ml. she was discharged after 48 hours and the postoperative period was uneventful. β-hCG levels showed a decreasing trend and became negative after 2 weeks.
Case 4
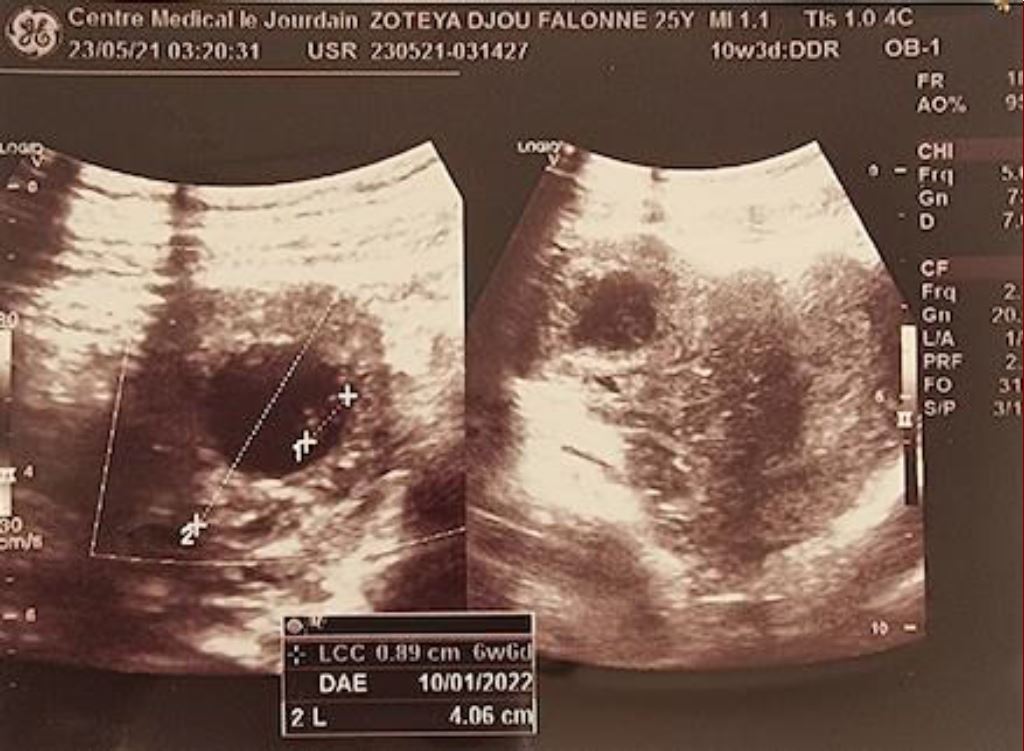
A 21-year-old woman, gravida 2, para 1, 10 weeks 3 days amenorrhea, was addressed by her gynecologist for laparoscopic management of an unruptured ectopic pregnancy. She presented to him with vaginal bleeding in the past 2 days with amenorrhea. Transvaginal ultrasound showed a right non-ruptured tubal ectopic pregnancy (Figure 5) and β-hCG level was at 7 375,65 mUI/ml.
Her Fernandez score was assessed at 13, indicating the necessity of surgery for her management. She underwent laparoscopic surgery and we found unruptured right interstitial pregnancy which required cornual resection and ipsilateral salpingectomy according to our protocol (Figure 6). The surgery lasted 65minutes and blood loss was 100 ml. she was discharged after 24 hours.
Discussion
Interstitial pregnancy occurs in the intra mural portion of the fallopian tube, being 0.7mm wide and 1 to 2 cm long (1). The vascularization network of this area is rich, originating both from ovarian vessels and uterine artery. Even if it is though that rupture occurs usually as late as after 12 weeks (1), this can happen earlier. In the presented data, rupture presented at 6 weeks in case number 2 with 2000 ml of hemoperitoneum, although the fact that myometrial distensibility tends to allow this pregnancy to present late. Because of cataclysmic hemorrhage, maternal mortality rate associated with ruptured interstitial pregnancy is 2 to 3% (6).
Ipsilateral salpingectomy appears to be the risk factor that is unique to interstitial pregnancy (7). Other risk factor includes uterine anomalies, past pelvic inflammatory disease, previous tubal and pelvic surgery, the use of assisted reproductive techniques and ipsilateral salpingectomy. In our case, risk factors found were Pelvic inflammatory disease (case 1), the use of morning after pills in two patients (case 1 and 3).
No risk factor was found in two cases. The diagnosis of interstitial pregnancy is a dilemma with many pitfalls. The difference between an interstitial pregnancy and an eccentrically located intrauterine pregnancy can be ambiguous (8). The use of transabdominal and transvaginal ultrasound to identify an empty uterus, a gestational sac seen less than 1 cm from the lateral edge of the uterine cavity, a thin myometrial layer surrounding the sac, and the presence of the interstitial line sign has been reported to improve the rate of diagnosis (9). The interstitial line has 80% sensitivity and 98% specificity for sonographic diagnosis of interstitial pregnancy. This important ultrasound diagnostic criterion is described as an echogenic line that extends into the upper regions of the uterine horn and borders the margin of the intramural gestational sac (8). Mapping of location of the pregnancy with three dimensional multiplanar sonography is a recent technique with more accuracy because it can more clearly delineate the intramural portion of the fallopian tube as it traverses the myometrium (10). Although much more accurate in the diagnosis of an early interstitial pregnancy than other imaging modalities, the higher cost of MRI makes it most appropriate for evaluation of cases in which ultrasound scans have been inconclusive (11). In our series, ultrasound was applied in 3cases and none of them clearly demonstrated interstitial pregnancy. This highlights the difficulty to diagnose interstitial pregnancy in our setting and the fact that radiologists have to be trained in an attempt to improve diagnostic accuracy. In our experience, laparoscopy is still reliable diagnostic tool, because it corrected the ultrasound diagnosis in all cases.
There are various medical and surgical treatment modalities for interstitial pregnancy. Although treatment with methotrexate requires a certain period of time with a potential risk of uterine rupture, the success rate of medical treatment varies from 70% to 90% according to some authors (12, 13, 14). It seems that gestational sac with a diameter greater than 2 centimeter is associated significantly with failure of non-surgical treatment (12) which is contraindicated in cases of heterotopic pregnancy with intrauterine pregnancy and interstitial pregnancy (15).
Traditionally, surgical treatment was performed by laparotomy with cornual resection or hysterectomy. Today, laparoscopy is the gold standard for treatment in ectopic pregnancy. In case of interstitial pregnancy, laparoscopic techniques involve cornuostomy as conservative method and cornual wedge resection plus salpingectomy for radical treatment (16). According to Tulandi (17), cornuostomy is appropriate for gestational sac diameter less than 3.5 cm, whereas Grobman and Milad (18) recommended cornual wedge resection when this diameter is more than 4 cm.
In our series, all patient underwent laparoscopic wedge resection and retrograde ipsilateral salpingectomy instead of conservative technique. Rupture occurred in two patients, so it was reasonable for us to be radical. For the three remaining unruptured cases, remaining conservative would require monitoring of Beta HCG while patients are economically limited, with a non-negligible failure rate given the size of the gestational sac. Even in women with significant hemoperitoneum, laparoscopic surgery can be safely conducted by experienced laparoscopic surgeons if hemodynamic stability is achieved by preoperative management (19). In our series, Laparoscopy lasted an average of 64.4 16 minutes and purse-string suture around the mass was performed in all cases and blood lost due to this procedure was 130 75 ml. Several hemostasis techniques using expensive equipment have been described in the literature (20, 21, 22). With a simple suture and skill in laparoscopic suturing principles, surgeons can realize purse-string suture to control the hemostasis, making the procedure becoming near bloodless.
Conclusion
Interstitial pregnancy is a life threaten situation which is fortunately a rare event. It poses a real diagnostic and therapeutic challenge. Control of the bleeding and removal of the ectopic pregnancy are the most important surgical principles. Laparoscopic approach with purse-string suture technique to control bleeding is suitable alternative to laparotomy and is ideal for surgeons skilled with principles of laparoscopic surgery and suturing.
References
Figure 1: Laparoscopic view of right unruptured interstitial ectopic pregnancy with encircling suture around the mass
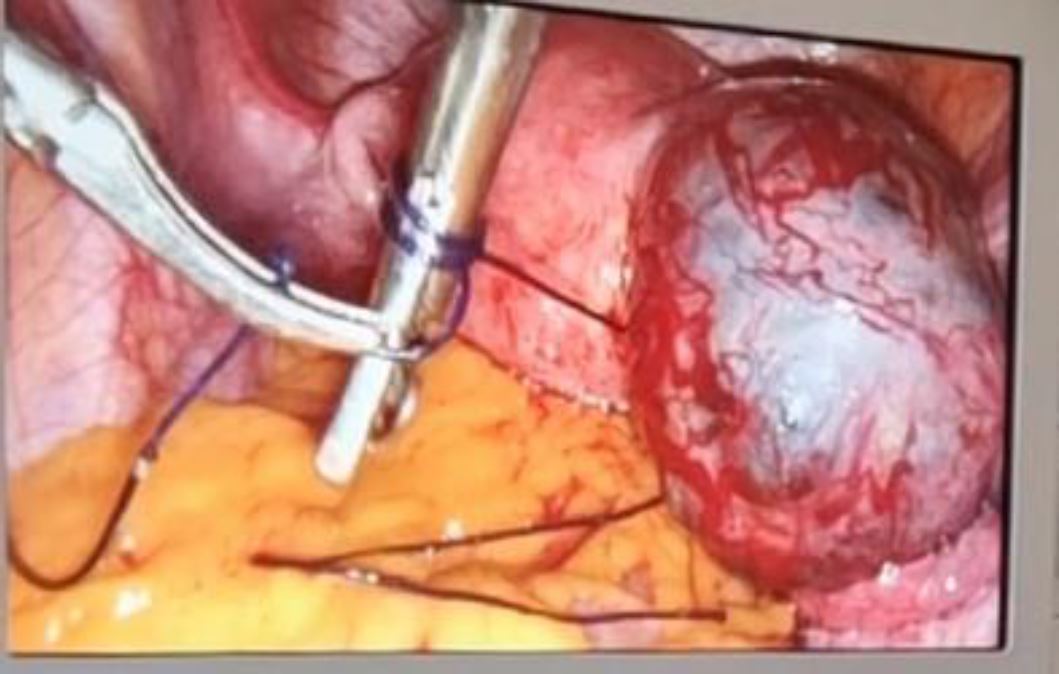
Figure 2: left ruptured interstitial ectopic pregnancy while controlling hemostasis with suture around the mass
Figure 3: Controlling hemostasis with suture around the mass before cornual resection of a left unruptured interstitial ectopic pregnancy
Figure 4: Final view after cornual resection and ipsilateral salpingectomy
Figure 5: Ultrasonographic view
Figure 6: Laparoscopic view of suture surrounding the mass