Authors / metadata
DOI: 10.36205/trocar1.2023004
Abstract
During last years, many innovations have been adopted in order to minimize the pain experienced during office hysteroscopy and to increase its completion rate, such as technical improvements, better tools and several pharmacological and non-pharmacological methods. Up to date, there is still no universal consensus about the most effective way to minimize discomfort during hysteroscopy. This chapter summarized the current recommendation and the most recent clinical data about the reduction of pain and discomfort during and before office operative hysteroscopy, highlighting the pharmacological and non -pharmacological measures.
Introduction
Hysteroscopy is a common and valuable intervention to diagnose and treat gynaecological conditions arising in the uterus such as infertility, abnormal uterine bleeding and suspected endo cavitary pathologies [1]. Biopsy of the endometrium in case of endometrial anomalies represents another diagnostic purpose of this technique. The outpatient setting in hysteroscopy is also proved to give several advantages, such as: avoidance of general anesthesia, shorter recovery time with immediate return to work or daily activities, higher patient satisfaction and it is more cost-effective. Although in most of women the outpatient hysteroscopy is well tolerated, the pain is still reported as the main limiting factor to the widespread use of this procedure by several papers about the acceptability of this procedure. The most important risk factors associated to pain and discomfort are nulliparity, menopause, presence of cervical synechiae and long operative time. On the contrary, patients who had at least one previous vaginal delivery seem to have a best tolerance to the procedure. During last years, many innovations have been adopted in order to minimize the pain experienced during this procedure and to increase its completion rate, such as technical improvements, better tools and several pharmacological and non-pharmacological methods. Up to date, there is still no universal consensus about the most effective way to minimize discomfort during hysteroscopy.
This chapter summarized the current recommendation and the most recent clinical data about the reduction of pain and discomfort during and before office operative hysteroscopy, highlighting the pharmacological and non -pharmacological measures.
Pathophysiology of pain during hysteroscopy
The nociceptive signal concerning intraperitoneal structures is conducted to T12-L2 spinal ganglia by visceral afferent fibers through both inferior and superior hypogastric plexus. The passage of the hysteroscope into the cervical canal, the uterine cavity distension, and peritoneal irritation due to spill of fluid into the abdomen are reported as the main responsible for pain originating during hysteroscopy. On the contrary, the increase in prostaglandins production due to endometrial damage is advocated by some authors as the cause for the delayed pain after 30 min from the procedure [2].
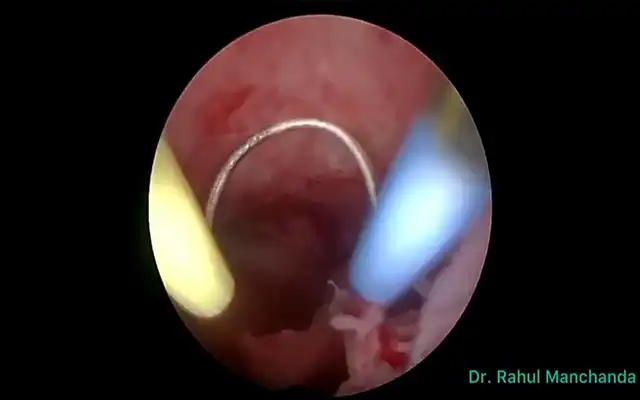
Vaginoscopy technique
Diagnostic hysteroscopy should be performed following the “no touch” approach to reduce the discomfort of the patient. This approach consists of inserting of hysteroscope into the vagina under visual control without touching the labia and vaginal walls [3]. It is well established that the introduction of hysteroscope by vaginoscopy provides less pain when compared to the use of speculum and tenaculum [4]. The use of smaller instruments (3.5 mm vs 5 mm) is also associated to reduction in painful experience as reported by several series with a lower pain score at the visual analogue scale (VAS), especially in nulliparous and menopause subgroups [5,6]. The use of a distension medium during the procedure is necessary since the uterine cavity is a virtual space which requires to be distended. To date, the saline solution media is considered superior to CO2 according to the intensity of pain perception, incidence of shoulder pain and patient’s satisfaction as described in the metanalysis of Craciunas et al. [7]. This is probably related to the easier insertion of instruments through cervical canal when saline solution is used [5]. The use of CO2 was also associated to most frequent side effects such as vasovagal reaction, bleeding and shoulder pain.
These results appear in contrast with most recent data published by Mazzon et al. and Tagliaferri et al. in which the women that underwent hysteroscopy with CO2 experienced a significant lower pain [6,8]. The reasons of these findings was explained by the significant shorter time of hysteroscopy performed with carbon dioxide. Several studies were also conducted on the relation between pain and pressure or temperature of fluid distension media used during diagnostic hysteroscopy [9,10]. Higher pressure (> 70 mmHg) seems to be responsible for an increase in pain experience during the procedure due to sudden distension of uterine walls. On the other hand, the pressure levels is not related to an increase of pain perception 30 minutes after the procedure [9]. For this reason, the operator should start the diagnostic hysteroscopy with lower pressure and gradually increase it until an adequate vision is reached. Regarding the temperature, the use of warmed saline solution was not effective in reducing discomfort compared to saline at room temperature [10].
Regardless the diameter of instruments or characteristics of distension media used, performing a correct technique to reach the uterine cavity is considered the most important factor in pain experienced by patients. Particularly, the passage of hysteroscope through the cervical canal is reported as the most painful step of the procedure. In order to reduce the pain it is of the utmost importance the correct placement of the hysteroscope in the cervical canal which should avoid to touch the cervical wall.
Pharmacological treatment
Anesthetic drugs
Various methods of analgesia have been reported in literature to suppress the pain associated with hysteroscopy. In a recent meta-analysis including 2610 patients De Silva et al. showed that all routes of administration including topical application (to the ectocervix and / or transcervical instillation) and injection (intracervical, paracervical and intracornual blocks) of lidocaine, mepivacaine, prilocaine and bupivacaine achieved a statistically significant reduction in pain during office hysteroscopy. However, mepivacaine and bupivacaine were the only specific local anesthetics that produced a statistically significant reduction in post-procedural pain scores [11]. Similarly, in the meta-analysis by Cooper and coll. was reported that paracervical and intracervical injection of local anesthetic drugs reduced pain during outpatient hysteroscopy and the meta-regression analysis showed that paracervical injection was significantly more effective than the other methods. In contrast, the intracavity instillation of local anesthetic and anesthetic applied topically to the cervix did not substantially reduce the pain during the procedure [12]. In line with these results in randomized, double-blind, placebo-controlled trial the application of lignocaine gel 2% to the cervix during outpatient hysteroscopy was not effective in reducing overall pain and pain in any individual step of the procedure compared to the placebo [13]. According to literature data, the instillation of intrauterine lidocaine injected directly to the cervix or given as a paracervical block few minutes before the procedure would seem to be associated with the reduction of pain during the procedure, however the act of intrauterine instillation of lidocaine can be painful. For this reason many authors have researched an alternative anesthetic methods. In a recent study 10 mL of lidocaine 2% added to 1000 mL of saline solution was used as the distension medium. The study group had an average rise of 1.9 in the VAS score after the procedure compared with 2.9 in the control group (p = 0.033). There was also a nonsignificant trend for shorter duration of hysteroscopy in the intervention group compared with the control group (180.1 vs 222.1 seconds, p = 0.08) and no side effects were recorded in either group [14]. In contrast, the use of sublingual buprenorphine for pain relief in office hysteroscopy has not shown encouraging results.
The tablet of buprenorphine 0.2 mg had no benefit in reducing the pain associated with hysteroscopy and was associated with adverse effects (e.i. drowsiness, nausea or vomiting) and a lower level of satisfaction [15].
Prostaglandins for cervical preparation
Currently there is insufficient evidence to recommend routine mechanical cervical dilatation prior to outpatient hysteroscopy, especially in the context of modern miniature hysteroscopes which avoid this unnecessary step. Regarding the relationship between the use of cervical preparation with prostaglandins and the reduction of pain during hysteroscopy discordant results are reported in literature. In a randomized, double-blind, placebo-controlled clinical trial by Nakano et al. including 158 postmenopausal women, 79 of these received 200 mg of vaginal misoprostol before diagnostic hysteroscopy. The procedure was performed by a rigid hysteroscope, based on a 2.9-mm rod-lens system with a 30° foroblique view, a Pozzi tenaculum forceps was used to grasp the uterine cervix and carbon dioxide was used as the distension media with a 50 to 60-mm Hg flow that did not exceed 100 mm Hg. The authors reported that the use of misoprostol did not reduce pain intensity neither the duration of the procedure and was associated with adverse effects, such as genital bleeding, abdominal cramping pain, and diarrhea [16]. On the contrary, in a similar study the authors included 100 postmenopausal patients (n. 50 = control group; n. 50 = study group) and the use of vaginal dinoprostone 3 mg administered 12 hours before diagnostic hysteroscopy was significantly correlated to the reduction of the intensity of pain. The procedure was conducted by a vaginoscopic approach without speculum and tenaculum, using a rigid 30˚ angled, 2.9-mm hysteroscope with a 4-mm outer sheath, normal saline was used to distend the uterine cavity, and the intrauterine pressure was maintained at 50 mmHg with an electronically controlled pump to prevent excessive distension of the uterine wall [17]. Similar results were reported in the study by Inal et al., which demonstrated the superiority of 10 mg vaginal dinoproston over 400 μg vaginal misoprostol administered 6 to 8 hours before diagnostic hysteroscopy in nulliparous women inducing more cervical priming and increasing cervical width before the procedure [18].
Antispasmodic and pain medications
Antispasmodics are commonly used in outpatient gynecologic procedures due to their specific action on the cervical–uterine plexus, reducing spasms achieved by cervical smooth muscle cells and at the same time acting as a bland cervical dilator. In a randomized controlled trial by Sharma et al. the antispasmodic drotaverine, administered orally with mefenamic acid before in-office hysteroscopy and endometrial biopsy, was compared to paracervical block achieved with 1% lignocaine. The oral drotaverine plus mefenamic acid was more effective than paracervical block in reducing pain perception [19]. Moreover, in a recent randomized double-blind placebo-controlled trial the oral antispasmodic hyoscine butyl-bromide (HBB) was not effective as the oral diclofenac potassium in the reduction of pain perceived by the patients undergoing office hysteroscopy [20]. Intramuscular injection of phloroglucinol improved the cervical width throughout a wider dilatation, helping to gain an easier cervical passage and reducing pain and discomfort. This route of administration represents an alternative to oral or vaginal misoprostol, with lower side and adverse effects [21]. The use of pre-medication with non-steroidal anti-inflammatory drugs (NSAIDs) or paracetamol was also investigated over the past years. The use of mefenamic acid administered before outpatient hysteroscopy was investigated and any significant lowering in patient discomfort during or after the examination was reported [22]. A 2017 Cochrane analysis evaluated that there are insufficient data to prove their effectiveness in obtaining pain reduction during the examination [23]. On the other hand, a trial by Abbas et al. showed that the use of oral diclofenac potassium, scheduled one hour before in office hysteroscopy, significantly reduces the discomfort, shortening the procedure time and increasing the level of toleration, when compared to the antispasmodic hyoscine butyl-bromide [24]. In a prospective randomized study the administration of 1 g paracetamol and 600 mg ibuprofen one hour prior to office hysteroscopy was not statistically related to decrease of pain experienced during the test, as well as 5 and 30 minutes after its completion, as assessed by the visual analog scale. However the occurrence of side effects such as nausea, emesis, and hypotension decreased statistically in patients who received analgesia [25]. In addition, the administration of rectal indomethacin has been found effective in reducing pain perceived during office operative hysteroscopy [26]. In a randomized double-blind placebo-controlled trial the use of Celecoxib, a selective cyclooxygenase-2 inhibitor administered orally, was investigated. The use of Celecoxib 200 mg was related to reduction of pain compared to placebo and it was found not inferior to oral Tramadol 100 mg in reducing discomfort or pain during office hysteroscopic surgery [27].
Non-pharmacological measures
Intra-operative music
Regarding non-pharmacological management, several studies evaluated the effectiveness of music in reducing anxiety and pain perception during office hysteroscopy. The randomized controlled trial by Mak et al. showed no positive effect of music regarding pain (p=0.382), anxiety (p=0.491) or satisfaction (p=0.165) [28]. A recent prospective randomized controlled trial conducted on 107 patients (music group n. = 54; control group n. = 53) showed that patients in the music group experienced significantly less pain during outpatient hysteroscopy (VAS score 4.54 ± 2.89 vs 5.88 ± 2.90; P = 0.02). The vital parameters measured before and during hysteroscopy, secondary outcome of the study, were not statistically significantly different between the two groups [29]. The prospective randomized trial by Angioli et al. that enrolled patients undergoing office hysteroscopy using the vaginoscopic approach without any type of anesthesia, reported that women in the music group experienced significantly lower anxiety and less pain during the procedure, and a significant decrease in both anxiety and pain scores after hysteroscopy (p<0.001) [30]. In summary, there is some evidence that music is effective in controlling pain and anxiety during hysteroscopies.
Transcutaneous electrical nerve stimulation
Transcutaneous electrical nerve stimulation (TENS) consists of the application of a pulsed electrical current through the skin using surface electrodes, a non-invasive form of analgesic treatment. In literature four studies have specifically studied the analgesic effect of TENS during hysteroscopy. De Angelis et al., in 2003, concluded that women assigned to the TENS group experienced significantly less pain than those in the control group [31]. Yilmazer et al., in 2012, studied the effect of TENS in women who underwent a hysteroscopy with biopsy in conjunction with an oral pharmacological treatment. Women reported a significant reduction in the pain they experienced compared to the placebo group 15 min after the procedure [32]. Lison et al., in 2017, showed a significant decrease in the mean pain score among patients in the active TENS group CLIMACTERIC 5 compared to the control group, at every stage of the hysteroscopy procedure [33]. Wang et al., in a randomized controlled trial published in 2022, showed that wearable transcutaneous electrical acupoint stimulation bracelet is related to prevention of postoperative nausea and vomiting in patients undergoing hysteroscopy [34]. According to these studies, this technique, if appropriate TENS parameters are selected so that the proper electrical stimulation dose is applied, can be useful for reducing pain during hysteroscopies because it is clinically effective, non-invasive, and without contraindications.
Hypnosis
Some authors have reported a correlation between the hypnosis and the reduction of pain during hysteroscopy. In a meta-analysis of Schnur et al. hypnosis use reduced discomfort, moreover it had a significant effect on anxiety and pain, some critical limits for the satisfactory completion of hysteroscopy [35]. In a retrospective study conducted by Gauchotte et al. no significant differences were found between the group undergoing to hypnosis and the control group in terms of pain, either during or after the procedure [36]. However, in this study the procedures are limited to hysteroscopic tubal sterilization. In addition, because this was a retrospective study, its conclusions are limited. Randomized controlled studies are needed to better investigate this method.
Viewing the screen during a hysteroscopy procedure
Two studies assessed the impact of the vision of the screen during the hysteroscopy on patient’s experience. In the randomized trial by Ogden and coll. 157 women undergoing office hysteroscopy were randomly allocated to vision of the screen (n = 81) or not (n = 76). The authors concluded that no significant positive effects are related to the vision of the screen and this may interfere with the patient–physician interaction [37]. On the other hand, Morgan et al. reported that in a group of 30 women undergoing hysteroscopy 10 of these wanted to watch the monitor during the procedure and they said that this solution took their mind off the pain [38].
The vocal–local approach
The vocal–local approach is based on the concept that empathetic attention to the patient is able to reduce pain and discomfort related to the procedure. During the hysteroscopy the operator and the supporting staff should provide emotional support to the woman to reduce the level of anxiety and may also involve the patient directly in the procedure. Evidence shows that a comfortable approach that involves the women directly in what is happening during the gynecological procedure might be able to act increasing patient satisfaction and reducing the need for pharmacological treatments [39]. In accordance with the good practice of pain relief and informed decision making for outpatient hysteroscopy by Royal College one member of the team should be exclusively dedicated to looking after the woman’s immediate needs and overall wellbeing rather than concentrating on the technical elements of the procedure [1].
Conclusion
Outpatient hysteroscopy represents a common diagnostic and therapeutic intervention in contemporary gynecological practice. This procedure is well tolerated by the majority of patients, however some women reported distressing experience, due to pain during and before the hysteroscopy. It is generally accepted that the use of the smallest diameter hysteroscopes, the vaginoscopic “no-touch” approach and the low inflow and distention pressures has reduced the discomfort and pain experienced during the procedure. However these measures may not be enough, particularly in nulliparous and postmenopausal patients. The use of local anesthetics through paracervical infiltration appears to be effective, as well as lidocaine added to saline solution used as distension medium. Regarding the usefulness of cervical preparation with prostaglandins prior to the hysteroscopy, the dinoproston appears to be significantly correlated with reduction of the intensity of pain. Also the use of pre-medication with non-steroidal anti-inflammatory drugs (NSAIDs) or paracetamol or antispasmodics drugs is related to the reduction of discomfort and other side effects such as nausea, emesis and hypotension. Particularly, the administration of rectal indomethacin or oral celecoxib has been found effective in reducing pain perceived during office hysteroscopy.
Moreover, the use of non-pharmacological measures, including music, transcutaneous electrical nerve stimulation and the communication with the patient prior and during the procedure are useful in reducing the anxiety level and discomfort or pain experienced by patients undergoing outpatient hysteroscopy.
However, it is mandatory to screen and identify patients who are at higher risk of high levels of pain experience during office hysteroscopy (i.e. nulliparous or postmenopausal women or patients with a stenotic cervix), in order to choose the most suitable aid to make the procedure more tolerated.