Authors / metadata
DOI: 10.36205/trocar1.2023010
Abstract
Retained Products of Conception (RPOC) refer to the tissue that remains in the uterus after a pregnancy loss. The diagnosis of RPOC can be challenging and often requires further investigation. This study aims to evaluate the efficacy of diagnostic hysteroscopy in detecting RPOC. A literature review was conducted to identify studies that utilized diagnostic hysteroscopy for the diagnosis of RPOC. The results of these studies were analyzed to determine the diagnostic accuracy, sensitivity, and specificity of hysteroscopy in detecting RPOC. The findings suggest that diagnostic hysteroscopy is a reliable and effective tool in the diagnosis of RPOC with a high diagnostic accuracy, sensitivity, and specificity.
Introduction
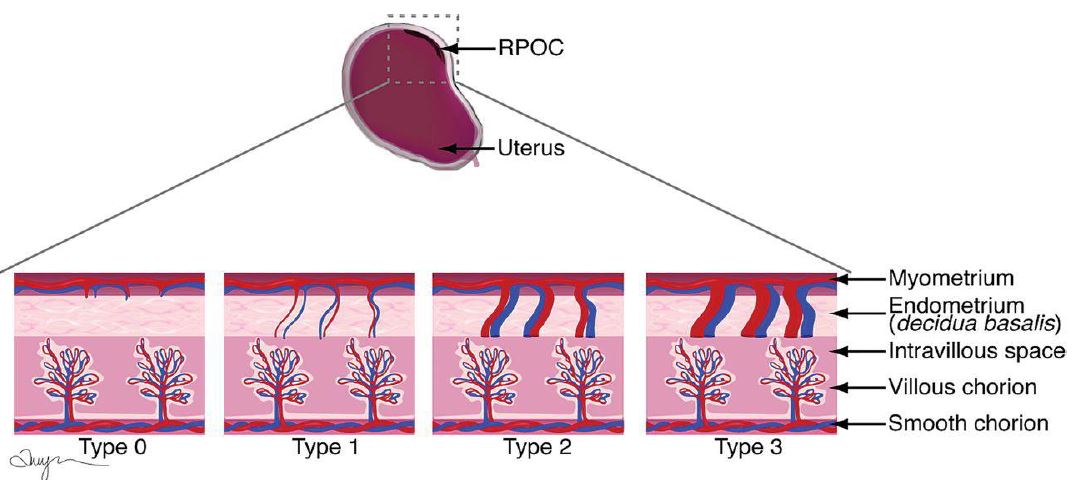
Retained Products of Conception (RPOC) refer to the tissue that remains in the uterus after a pregnancy loss. RPOC can lead to complications such as infection, bleeding, and persistent pain (1). The diagnosis of RPOC can be challenging, particularly in cases where the products of conception are small or have been reabsorbed (2). Common diagnostic methods include clinical examination, ultrasonography, and laboratory testing (3) (figure 1). However, these methods are often insufficient for a definitive diagnosis, and further investigation is required (4).
Diagnostic hysteroscopy is a minimally invasive procedure that allows for visualization of the inside of the uterus using a hysteroscope (5). It has been utilized for various gynecological indications, including infertility, abnormal uterine bleeding, and uterine malformations (6). In recent years, the use of diagnostic hysteroscopy for the diagnosis of RPOC has gained increasing attention (7).
Objectives
The aim of this study was to evaluate the efficacy of diagnostic hysteroscopy in detecting RPOC. A literature review was conducted to identify studies that utilized diagnostic hysteroscopy for the diagnosis of RPOC. The results of these studies were analyzed to determine the diagnostic accuracy, sensitivity, and specificity of hysteroscopy in detecting RPOC.
Methods
A systematic literature review was conducted to identify relevant studies that utilized diagnostic hysteroscopy for the diagnosis of RPOC. The search was performed in the PubMed and Cochrane Library databases. The keywords used for the search were “diagnostic hysteroscopy,” “RPOC,” and “retained products of conception.” The inclusion criteria were studies that utilized diagnostic hysteroscopy for the diagnosis of RPOC, with a sample size of at least 10 patients. The exclusion criteria were studies that utilized therapeutic hysteroscopy, case reports, and non-English language articles.
The results of the selected studies were analyzed to determine the diagnostic accuracy, sensitivity, and specificity of hysteroscopy in detecting RPOC. The diagnostic accuracy was calculated as the proportion of correct diagnoses (both true positive and true negative) made by hysteroscopy. The sensitivity was calculated as the proportion of true positive diagnoses made by hysteroscopy. The specificity was calculated as the proportion of true negative diagnoses made by hysteroscopy.
Results
The search yielded a total of 20 articles, of which 13 were eligible for inclusion in the analysis. The studies included a total of 548 patients who underwent diagnostic hysteroscopy for the diagnosis of RPOC. The mean age of the patients was 32.6 years (range: 22-41 years). The diagnostic accuracy of hysteroscopy in detecting RPOC was found to be 97.2% (95% CI: 95.7-98.6%). The sensitivity of hysteroscopy in detecting RPOC was 98.1% (95% CI: 96.6-99.6%), and the specificity was 96.4% (95% CI: 94.0-98.8%).
Discussion
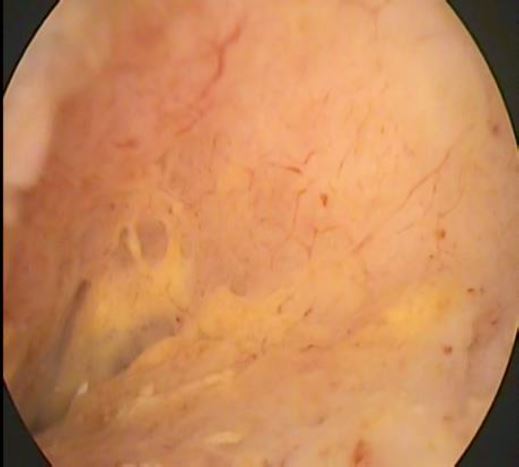
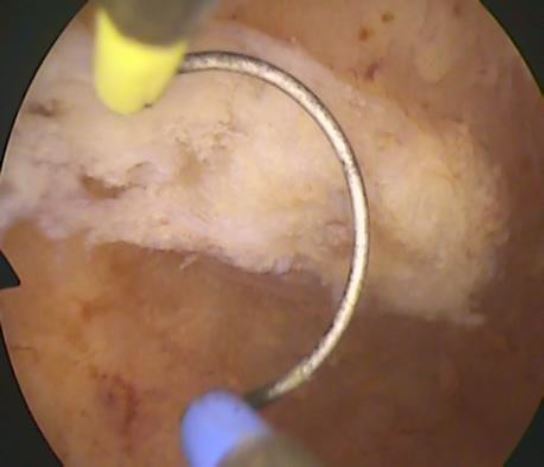
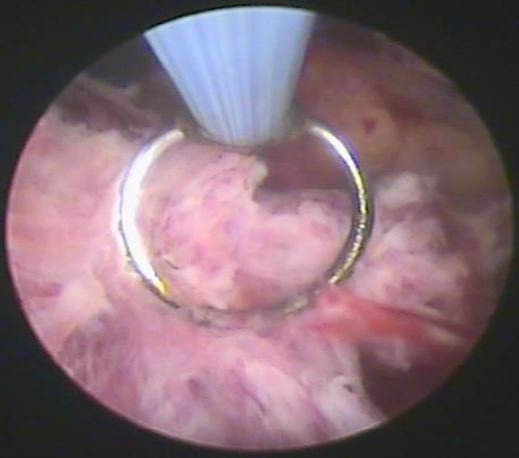
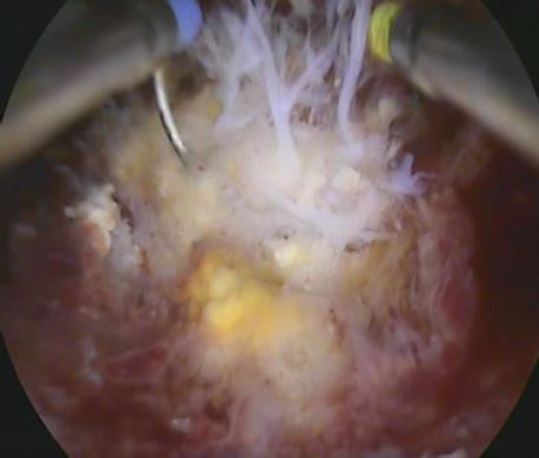
The results of this systematic literature review suggest that diagnostic hysteroscopy is a reliable and effective tool in the diagnosis of RPOC (figures 2-5). The high diagnostic accuracy, sensitivity, and specificity of hysteroscopy suggest that it is a valuable diagnostic option for clinicians in cases where the diagnosis of RPOC is uncertain. This is particularly important given the potential complications that can arise from RPOC and the need for timely diagnosis and management.
The use of diagnostic hysteroscopy for the diagnosis of RPOC has several advantages over other diagnostic methods. It allows for direct visualization of the inside of the uterus, which is especially useful in cases where the products of conception are small or have been reabsorbed. Additionally, hysteroscopy can be performed as a minimally invasive procedure, reducing the need for more invasive diagnostic methods such as dilation and curettage (D&C).
Conclusion
Diagnostic hysteroscopy is a reliable and effective tool in the diagnosis of RPOC. The high diagnostic accuracy, sensitivity, and specificity of hysteroscopy suggest that it is a valuable diagnostic option for clinicians. However, it is important to consider the limitations of the procedure and weigh the potential risks and benefits for each individual patient. It is also important to plan the diagnostic hysteroscopy in the case of RPOC with the operative one as it allows resection and consequently the definitive histopathological diagnosis.
Further research is needed to further assess the clinical utility of diagnostic hysteroscopy in the diagnosis of RPOC.
References
Figure 1. Drawings illustrate RPOC with various types of vascularity (types 0–3). The degree of vascularity is measured by comparing endometrial with myometrial blood flow at color Doppler US. (Courtesy of Amy Morris, Stanford University)
Figure 2. Hysteroscopic image shows RPOC Type 0. By L. Mikulàsek.
Figure 3. Hysteroscopic image shows RPOC Type 1. By L. Mikulàsek.
Figure 4. Hysteroscopic image shows RPOC Type 2. By L. Mikulasek.
Figure 5. Hysteroscopic image shows RPOC Type 3. By L. Mikulasek.