Authors / metadata
DOI: 10.36205/trocar1.2023012
Abstract
Congenital anomalies of the female reproductive system are commonly seen in 4-6% of women. [1] These may be responsible for infertility and recurrent pregnancy loss. With the advent of three-dimensional (3D) ultrasound, many of these anomalies can be reliably diagnosed without performing any invasive techniques. Yet, hysteroscopy when combined with imaging provides a way to confirm the diagnosis and treat these patients with optimal reproductive outcomes.
This nonsystematic review article aims to define the role of hysteroscopy in diagnosis and classification of these anomalies, along with addressing some treatment dilemmas that arise when these conditions are encountered in every day practice.
Introduction
The prevalence of congenital uterine anomalies is reported to be 4.3–6.7% in the general population, 3.4%–8% in the infertile population, and 12.6–18.2% of those with recurrent miscarriages [1] According to the findings of this review the commonest anomalies follow the order of arcuate, septate and bicornuate at a ratio of approximately 17:7:1 [2] Septate uterus is the most common uterine anomaly in the infertile population (3.9%), while the arcuate uterus is the most common anomaly in the general population and in those with recurrent miscarriage. The prevalence of uterine septum and arcuate uterus in infertile patients varies in the literature, but it is estimated to be 3.9% and 2.1% respectively [2].
Classification
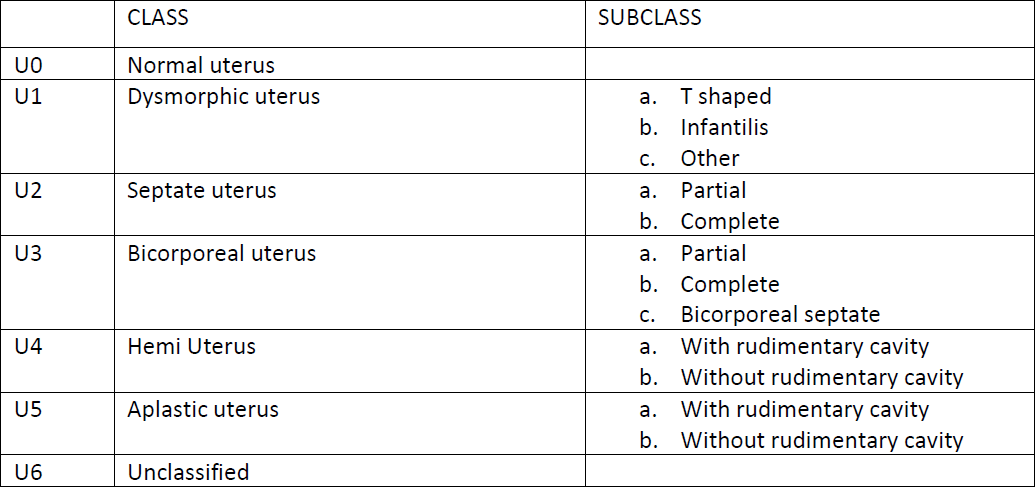
Congenital uterine anomalies are classified, according to the CONUTA classification from U0 to U6 according to the deformity [3] [table 1].
A variety of techniques has been utilized for assessing the uterine cavity such as hysterosalpingography (HSG), two dimensional (2D) trans vaginal sonography (TVS), saline infusion sonography, three dimensional TVS (3D TVS) and even magnetic resonance imaging (MRI) [4].
3D TVS, a new technique of imaging, has the ability to register all three imaging planes simultaneously as well as visualize the surfaces three dimensionally.[8,9] It thus provides a unique diagnostic tool for noninvasive visualization of the uterine morphology as well as the diagnosis of congenital uterine anomalies [4]. MRI also provides detailed information on the uterovaginal anatomy, particularly in the study of the external profile of the uterine fundus and the cavity shape, and it also allows visualization of the septum within the cavity.
Role of Ultrasonography (USG) and Magnetic Resonance Imaging (MRI).
The clinical and imaging diagnosis must be certain before proceeding with an invasive (even diagnostic) surgical intervention
Patient Preparation
The patient is preferably scheduled for surgery in the early proliferative phase of the menstrual cycle. This ensures that the endometrial lining is at its minimum thickness, and smaller shape defects like an arcuate uterus, or a unilateral convergent wall (the 7- shaped uterus) are not missed during the primary examination because of being obscured by the thick endometrium.
Hysteroscopy is best performed using a 2.9 mm or 1.9 mm hysteroscope that allows easy entry into the uterine cavity. The administration of vaginal misoprostol 400 μg, 4 hrs before the procedure may aid in an easy entry into the cavity, although there is no evidence to support its routine use in hysteroscopy [5].
Hysteroscopic approach
Entry
The preferred route of entry into the uterine cavity is by using the vaginoscopy- hysteroscopy technique. In patients undergoing an office procedure, this is the only available technique [6]. However, even in patients who are being operated upon under anaesthesia, performing a vaginoscopy – hysteroscopy and ‘entering under vision’ is equally important. This ensures that the entire vagina, its fornices and the cervical anatomy, along with the external os is clearly visualized before an entry is made into the cavity. This ensures that even minor defects are not missed out. Needless to say, vaginoscopy is an adjunct to, and does not replace a thorough per speculum and per vaginal exam.
Some of the anomalies/ abnormalities that could be detected at this stage are;
- Complete vaginal septum – associatedwith a complete uterine + cervicalseptum
Both halves of the vagina, and both hemicervices are inspected after distendingeach hemi vagina with the distensionmedium. The telescope is inserted ineach hemi cavity and both ostiavisualised - Transverse vaginal septum – possiblyassociated with agenesis of the lowercervix / upper vagina. A pinpoint openingof the transverse septum may be seen,though in most cases it is too small to benegotiated with a telescope
- Concomitant puckering and nodularity ofthe posterior fornix suggesting rectovaginal septum endometriosis –frequently associated with a noncommunicating functional hemi uterusand pelvic endometriosis
- A pinpoint external os – in patients withhypoplastic uterus
- Cervix completely flushed to the vaginalwall
The view from the internal os
Once the internal os has been negotiated, the first look into the cavity provides a wealth of information
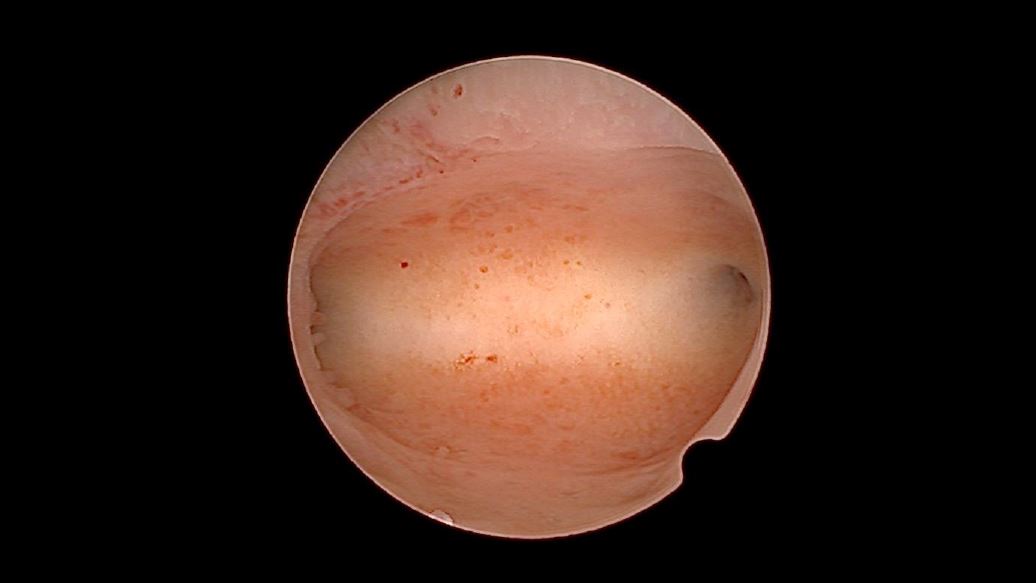
The surgeon must carefully inspect the fundus, lateral walls and both ostial openings from the vantage point of the internal os. On inspection, a ‘normal’ uterus should have the following features (fig 1)
- The fundus is usually curved slightlyinwards, rather than completely flat.Subsequently, the area between the twoostia appears slightly elevated andprojecting into the cavity
- The two ostia are equidistant from themidline
- Both ostia are seen in one single view(not a very consistent finding)
- If the two ostia are not seen together ina single frame, each ostium is at leastvisible from the internal os when thelight cable is tilted from the 6 O’clock tothe 3 and 9 O’clock positions
- The overall cavity appears ‘spacious’.This is a subjective assessment, learntover a period of time after performing anumber of cases
Any variations to this anatomy should raise the suspicion of a uterine anomaly. Of course, the hysteroscopy findings must complement, and not dispute the diagnosis that has been made on imaging pre operatively
- a.The Septate/ arcuate Uterus ( Class U2): Anyprojection of the fundus in the midline, equalto or more than one third distance from theinternal os to the fundus, can directly becalled a septate uterus (fig 2). Smallerindentations than this may be arcuate ratherthan septate. This is however, a subjectiveassessment and not nearly as reliable asmeasuring the depth of the septum inrelation to the myometrial thickness on 3DUSG, which is considered the gold standard.
There is no universally accepted technique of making objective measurements inside the uterine cavity. The graduated uterine palpator by Karl Storz is used at some centres [6]. The other way to get an approximate estimate of distance is using a hysteroscopic instrument (grasper or scissor).
The distance between the open jaws of the instrument is first measured outside the uterine cavity. Using this information, the total length of the septum is assessed during surgery without actually cutting the septum. Similar information can also be obtained by using the straight resectoscope loop [7].
There is consistent data indicating arcuate uterus as an acceptable variety of normal uterus, which does not need any surgical repair.
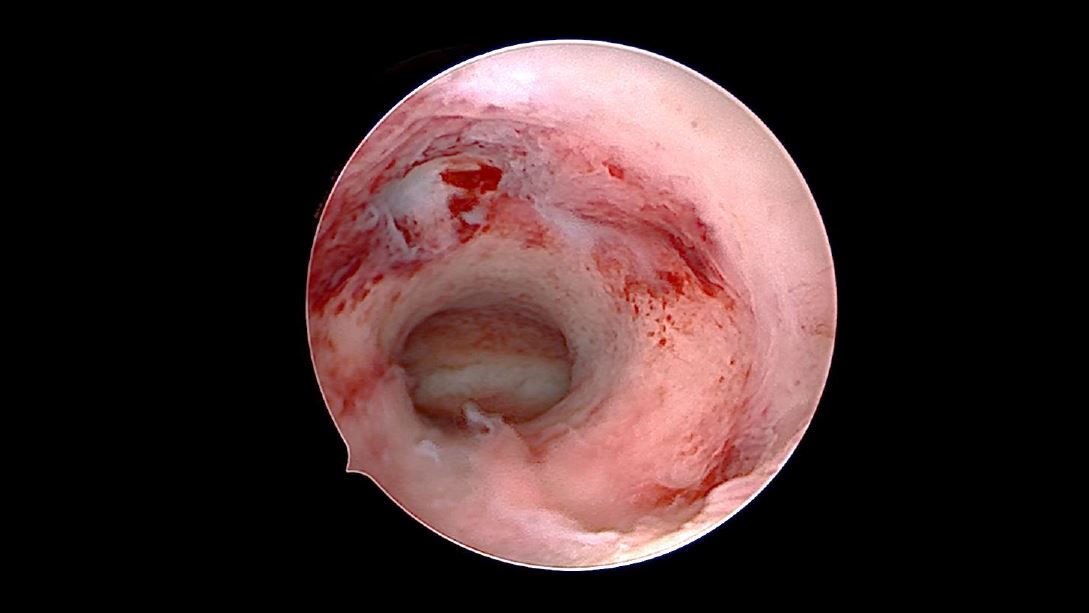
- b.The T shaped uterus (Class U1): a tubular,tunnel like cavity is seen beyond the internalos. Both tubal ostia are not visualised (fig 3).The telescope has to be advanced higher intothe uterine cavity, usually beyond half thedistance of the cavity. At this stage, tilting thelight cable allows visualisation of the tubal
ostium. In case of a unilaterally convergent wall (the 7 shaped uterus), the view of only one of the ostia may be hindered by the hypertrophied lateral wall, and the other ostium clearly seen from the internal os. Making this observation carefully at this stage is very important, because this is also considered as the end point of surgical correction once the lateral wall has been incised with an electrode or a scissor.
It is worthwhile to remember that a uterus which is hypoplastic may have a cavity that looks exactly like that of a T shaped uterus which is normal in size externally. The distinction between these two must be made on pre operative imaging by 3D ultrasound, because only the latter is a case justified to undergo surgical correction.
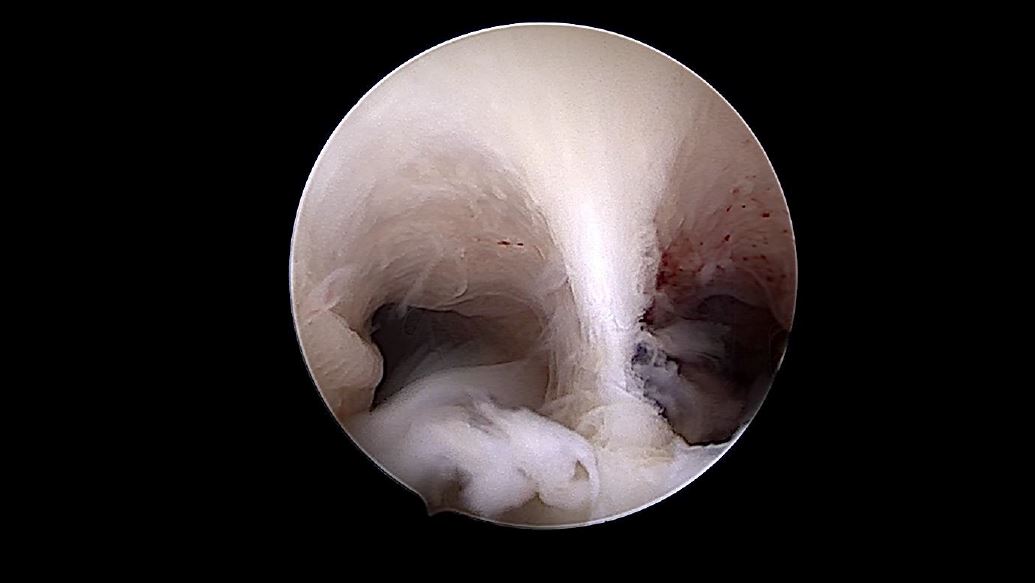
- c.The bicornuate uterus (Class U3): The cavityof a bicornuate unicollis uterus looks exactlysame as that of a completely septate uterus.It is very important to distinguish betweenthe two, because a casual septal incisioninitiated by just seeing an inward midlineindentation could result in a catastrophicperforation if the uterus is bicornuate, or bicorporeal septate, rather than septate. This distinction can be made pre operatively using a 3D ultrasound to define the degree of serosal indentation, or intra operatively by performing a concomitant diagnostic laparoscopy
- d.The unicornuate uterus (Class U4): a bananashaped, rather than a tubular cavity is seenwith a single terminal ostium. Obviously, thevolume of the cavity is reduced. The surgeonmust be careful to make sure that he/she hasnot missed the other half of a bicornuateuterus, and mistakenly visualised only onehalf of the cavity thereby labelling it as aunicornuate uterus. It is best to confirm thesize and functionality of the other horn by performing a simultaneous diagnostic laparoscopy
- e.The Accessory cavitated uterine mass(ACUM) (Class U6): Previously known asjuvenile cystic adenoma (JCA), ultrasoundleaves behind a diagnostic dilemma, confusing the entity with a functional non communicating uterine horn with hematometra. In both cases, the patient presents with severe dysmenorrhoea. In these cases, a diagnostic hysteroscopy performed before laparoscopy effectively rules out the possibility of a non-communicating horn, if both ostia are visualised.
- f.The Robert’s Uterus (Class U6): this conditionis also best diagnosed by pre operative pelvicMRI, and is an asymmetric fusion of thevaginal septum to one side of the midline.Consequently, hematocolpos andhematometra, sometimes hematosalpinxensues. On vaginoscopy, a bulge is seendistending one half of the vagina, and onlyhalf the circumference of the cervix is visible.The appearance of the uterine cavity, beforecorrective surgery is performed, is like a unicornuate uterus [8].
Conclusion
In summary, diagnostic hysteroscopy plays a vital role in both the diagnosis and management of congenital anomalies of the genital tract. Used in conjunction with clinical examination and imaging, hysteroscopy provides an invaluable tool for assessing and correcting these anomalies resulting in optimal surgical outcome.