Authors / metadata
DOI: 10.36205/trocar4.2022004
Abstract
Minimally invasive surgery has become the reference technique in several surgical specialties. Its penetration rate however remains low in countries with low economic resources. The causes of this deficiency are multifactorial. Economic causes and difficulties of access to specialized practical training represent the major obstacles to the development of this surgery. These failings are compounded by cultural prejudices and the lack of political will. To remedy this situation, health actors in these countries must innovate to facilitate learning and practice of minimally invasive surgery in low-resource environments. New technologies and communication tools can be of great help in bridging the economic gap. The adequate and appropriate use of local human and economic resources seems to be the key to success. In the long term, we will have to redefine a new custom made minimally invasive surgery adapted for situations with low human and economic resources.
Introduction
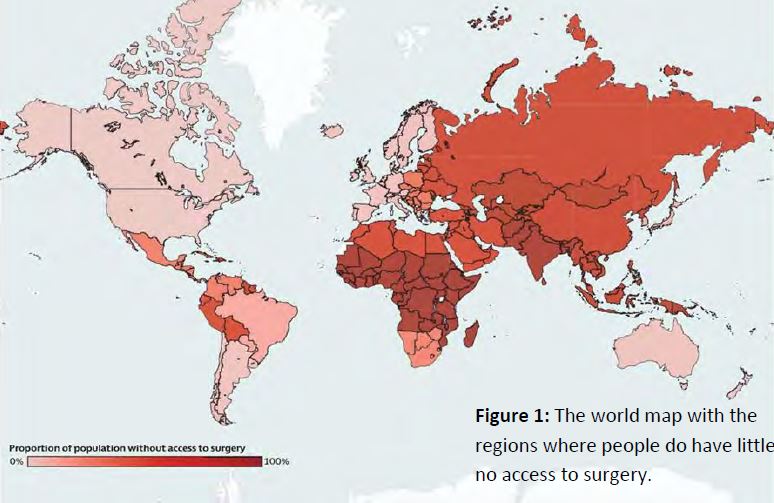
Surgical care plays a pivotal part in the health service. This universal right however is not available for everybody. In fact, in the Low-Income Countries (LICs) patients do suffer from the difficulty to access surgical care. On estimate, two third of the world population do not have access to reliable surgical care and two milliards of people do not have the possibility to receive surgical care. The latter is due to the lack of financial means and or human resources. This leads to the constatation that every year this limited access to surgical care kills nearly seventeen million human beings. This number exceeds the deaths caused by HIV/AIDS, tuberculosis and malaria combined (1-2) (Fig 1).
The economic inequalities of our planet reflect themselves manifestly in the health systems as 60 % of surgeries are realized for only 16% of the world population and only for 6% for the LIC’s population on the other hand, while one third of the world’s population lives in these countries. (3).
The High-Income Countries (HICs) do have better quality indicators and social security provisions. These do induce an increase of the cost for the social security. The increase of the costs of the social security in these countries grows more rapidly than their economy. This will necessitate a cut in the social security expenses to guarantee the quality of the social security in the future.
Minimal invasive surgery (MIS) has thrown a new light on classical surgery and did point to an evolution in the history of surgery. MIS does offer a magnified anatomy leading to better diagnosis and more accurate surgical gestures. MIS does allow for an efficacious treatment with a secured outcome respecting to the maximum the different organs and their function. The reduction in trauma to the abdominal wall and the peritoneum is associated with a lesser immediate postoperative discomfort; shorter hospital stays and shorter postoperative revalidation. The publication of these techniques by the pioneer units in the 1980-ties have led to the general application in a great number of interventions in several surgical specialties and have been adopted by most of the hospital units (4).
The technique has been largely adopted in the HICs. The situation is very much different in the LICs and Lower- Middle Income Countries (LMICs) countries. Its advantages do not have to be demonstrated in these countries where the hope is that these techniques will make it possible for more patients to have access to surgery. The aim of this revue is to make the point of the situation of MIS in the developing countries, to expose the obstacles of its development and to propose solutions for the future.
Actual status of surgery in the world
Despite the efforts deployed a large part of the world population remains having difficulties to access to quality medical treatment and therefore does, in concreto, not have access to the right on health services. Very important disparities still do exist between countries of the north and the south and between cities and rural communities (5).
According to the Lancet Commission on Global Surgery, at least 4,8 milliards of the global populations does not have timely access to reliable surgery (Fig 2). It is the poorest countries that encounter most difficulties to access to general treatment and especially to surgical treatment. On the one hand, more than 95% of the population in South Asia and in African Central Sub-Saharan both east and west do not have access to treatment whereas on the other hand only 5 % of the population of Australia, North America and Europe do not have access to treatment (6). The estimate is that in countries with low or intermediate income, nine out of ten people do not have access to basic surgical treatment and that 143 million of supplementary surgical interventions are necessary every year to prevent disability (7). Costs of surgery and anesthesia are at the origin of “catastrophic” expenses for some 33 million of people (8). The problem being essentially the burden of the direct costs concerning surgical treatment (9). Peri operative mortality is as high as 5 to 10% in the LICs versus 0,4 – 0,8% in the HICs, the majority due to infections, complications of anesthesia and per- or post-operative bleeding problems. The non-availability of equipment, infrastructure, medication and balanced organization are at the origin of these deficiencies (10). The HICs do have excellent indicators of quality and social security available, this is correlated with the high cost of health services and social security in these countries (11). The increase of the costs for health and social security in these countries is growing more rapidly than their economies. As an example, in the United States the costs for health and social security have risen rapidly and represent 17% of the Bruto National Product (BNP) (12). The consequences are that all over the world and more particularly in the LICs there is a need to reflect on ways to simplify the surgical care and make the latter more cost effective.
Actual Status of the Minimal Invasive Surgery (MIS) in the world
MIS in the developed countries
In almost all surgical specialties MIS has become mainstream over the last 20-30 years (13 -14). MIS has replaced conventional surgery for many indications. The reason being that MIS allows for reduction in patients discomfort, morbidity, reduction in prevalence of adhesions and also reduces hospital stay and enhances and shortens recovery for the patients (15-16). According to the American College of Surgeons (ACS), the use of laparoscopy is still increasing over the observed period of time from 22,7% in 2005 to 49,8% in 2014 (17). In Switzerland, a national study from 1998 to 2017 reveals that half of the colorectal resections have been realized by MIS in 2016 while cholecystectomies have been operated only by laparoscopy since 1998 (18). Less than one decade after the introduction of the laparoscopic technique, 500.000 to 600.000 cholecystectomies have been performed by laparoscopy in the United States only (19). Introduced by gynecology and still largely used in this specialty, laparoscopy is now used in digestive surgery (bariatric, gastrointestinal, colorectal and hepatic surgery) and in urology although technique covers just one aspect of MIS.
In its seventh report, Global Industry Analysts estimates that the global market in MIS has a value of 49 milliard of US Dollars in 2020 and will grow to 90,4 milliard US Dollars in 2027, meaning an annual growth of 9,1% in the period from 2020 to 2027. In the United States, the market of MIS was estimated to be 14,5 milliards US Dollars in 2020. In China, the second economy in the world, it is estimated that the MIS market will rise to 15,6 milliards US Dollars in 2027 powered by a yearly increase of 8,5 % up to 2027. Other remarkable geographical markets are Japan and Canada here the MIS markets will increase respectively of 8,7% and 7,3 % in the period from 2020 – 2027 (20).
MIS in the LICs:
The proven advantages of laparoscopy over “open air” surgery is even more important in the emerging countries especially in vue of the number of hospital beds, the scarcity of blood banks and the non-availability of modern imaging techniques (21). The technique in fact is perfectly adapted for use in the emerging countries as hospital stay is decreased and the return to normal activity for the patients is enhanced, factors that reduce the overhead costs for surgery. A major obstacle for the adoption of the technique in emerging countries is the non-existing official data and publications (22). Nevertheless, the few data available and published on the numbers of laparoscopic surgeries for gynecologic indications show that the numbers are very low and vary extremely from one hospital to the other (23). Published data in the large reference hospitals in different countries show that the prevalence of laparoscopic surgery for gynecologic indications remains under 10% (24). Furthermore, the use of laparoscopic techniques remains basic and in a series of centers restricted to only diagnostic procedures. The conclusion has to be that the adoption and the use of MIS in the emerging countries remains poor and that compared with “open air” surgery and only less complicated procedures are performed. (22).
Obstacles to the adoption of MIS:
The obstacles preventing the diffusion and adoption of MIS are multifactorial with as most important insufficient investments in surgical material and very specifically the sparsity of and difficulty to find specialized courses allowing to be trained in the technique (25). The sparsity of economic resources is the principal obstacle. The weak economic situation does not allow for the buying of endoscopic equipment nor the maintenance of the latter and the specific training of surgeons and technicians that would allow them to perform endoscopic procedures. The above explains why the use of endoscopy is mainly reduced to diagnostic procedures in the emerging countries (26). There is a direct relation between the bruto national product of a country on the one hand and the percentage of the complex MIS surgeries done on the other (25).
The relatively small number of surgeons in the LICs prevents them to subspecialize and this results in MIS being time consuming entities, mostly at the beginning, with potentially more complications that most of those surgeons are not able to handle (27). This creates an auto inhibitive effect causing the learning curve to become much longer. Furthermore, the surgeons and theatre personnel, well formed in MIS, are not always available. (28-29). The climate of limited resources in the LICs also hinders the training in laparoscopic skills due to the lack of experts willing to teach. Moreover, as soon as these experts are able to, they leave the university hospitals for more lucrative businesses. Another factor to deal with is the fact that the laparoscopic technique is not toughed in the third cycle of medical school in several LICs. The main reason being the lack of resources and therefore the teaching labs and simulation labs are difficult to find as the equipment is costly (30). This lack of training of the surgeons becomes apparent in the rate of conversion to laparotomy in the emerging countries as well as in a higher percentage of major complications and finally in longer operating times. (31-32-33) From the opinion of decision makers, surgery is traditionally evaluated to be complex and expensive. Surgery has never been included in the category of primary care although surgical interventions have proven to be of value in saving lives and preventing disabilities (34-35). Sometimes decision makers are hesitant and lack the will to take initiatives allowing for new perspectives as the adoption of the MIS in daily practice. Even more, some decision makers make statements declaring that MIS does not suit emerging countries due to the fact of the costs not only for the material but also for the training of the doctors and the necessity of a technical platform adapted to this form of surgery. Often “open air” surgery is considered to be more reliable in low resources environments (36). The last but not least obstacle is formed by sociocultural barriers as the older surgeons do resist changes (24). Some of these senior surgeons do represent a barrier to the development of MIS. In fact, they have more possibilities to be trained in MIS than their junior counterparts but they do not integrate MIS in their daily practice. They are suspicious towards new techniques and are not able to see the advantages of MIS due to a lack of information and appropriate training in MIS (37). All the above factors are aggravated by a bad management of the few available resources, financial and human, and the absence of a global vision on health and social security. The latter due to not knowing the actual health situation and the absence of objectives on the short and long term.
V Advantages of MIS in the emerging countries
Adapting MIS in emerging countries enables to generate several beneficial effects first clinical, but also economical and on a broader scale a positive impact on the social security and health situation.
1.Clinical advantages
- Reduced hospital stays
- Smaller abdominal scars andhence reduced risks oninfections
- Less long-term complicationssuch as eventrations andadhesions
- When there is a limitation inavailable imaging techniques,laparoscopy can reduce thenumber of unnecessarylaparotomies and can be helpfulin detecting pathologies liketuberculosis, intra-abdominalcancers, pelvic inflammatorydisease and abdomino-pelvictraumata (34).
2.Economic advantages
The adoption of MIS and laparoscopy in particular could be beneficial for the hospitals as compared with “open air” surgery
- Minimal use of analgesics,antibiotics, bandages and othermedical appliances (38).
- Shorter hospital stays (39 -40)
- Speedy return to the workplace.This is especially important inview of the impaired socio-economic conditions.
3.Structural advantages for the health systemand social security
In adopting MIS, more hospital beds will be available due to the more rapid discharge of the patients and this entails that the waiting time for surgeries can be reduced (41). Furthermore, laparoscopic schooling will give the surgeons a feeling of professional accomplishment and will give them motivation that in turn will inspire the patients to have confidence in the health system (42).
VI Future perspectives
Developing surgery and in particular MIS is imperative for emerging countries. In fact, 28% – 32% of the world’s morbidity can be brought back to pathologies that can be treated by surgery. It is also estimated that there will be an annual decrease of 2 % in BNP for the LMICs up to 2030 due to a shortage of surgery (43).
Surgeons will be called to play a primordial role in the orientations of the health politics in their respective countries as to guarantee reliable and universal treatments. The medicine and the surgery in the emerging countries at this moment in time are based on data coming in majority form HICs and adapted to the HICs economic, social and human conditions. This kind of medicine cannot just be transplanted in LMICs and LICs environments without being adapted before application.
The primordial role of the decision-making doctors in the emerging countries is to adapt– based on facts – this medicine, before application in their respective countries, to their own human and economic conditions without sacrifice nor security nor efficacy. This compromise between means and results is not easy but above all necessary. It requires from the medical decision makers an effort in innovation that at the moment is cruelly absent in these countries (22).
Adaptation of MIS in emerging countries
The adaptation requires a perfect knowledge of the actual data concerning the present practice of medicine and a thorough knowledge of the local economic, social and human conditions. The aim is to address both the technical part of care and the training of both doctors, paramedical personnel and technicians.
The specialized surgical techniques have to be reduced at their simplest form and made available to every surgeon, not time consuming, reliable with a reduced potential of complications and able to be performed with a minimum of instrumentation. The potential danger of a complication depends largely on the theatre environment where it arises. An ileostomy is easy to handle in a HICs but is potentially deadly in a LICs or LMICs.
Locoregional anesthesia should be used whenever possible especially in ambulatory surgery (44).
Preference should be given to reusable, easy to take apart and reassemble instruments. It is advisable for these instruments to be fabricated by local craftsmen and factories as this guarantees availability and stimulates local economy.
Surgical training has to be locally organized with the instrumentation locally used and under the same working conditions. Courses in the HICs with sophisticated instrumentations and expert techniques give rise to surgeons who will be torn between their rightful surgical ambitions and the local deceiving circumstances.
Adaptations described in literature contain:
- Gasless laparoscopy can be obtained byusing towel clamps or pieces of thread tobring tension on the abdominal wallusing a laparolift, a laparofan or poweractivator and abdominal retractor (45).
- Constructing alternatives for endobagsusing low-cost condoms, packaging ofnasogastric tubing’s or gloves (46 – 47 – 48).
- The use of reusable trocars andinstruments using a sterilizationprocedure, the use of drapes and tubesthat can be washed and autoclaved.These instruments have a live span of upto 18 years and allow for an economy ofup to $ 300 per surgery. (49-50-51-52)
- Use the sun as light source (53).
- Use simple instruments to skeletonisestructures (49).
- Use ovum forceps to make a stoneremover (49).
- Use a cystoscope as a laparoscope (50).
- Replace a harmonic scalpel with bipolarforceps’s (54).
- Make tripolar forceps with a knife inbetween the bipolar forceps (54).
Innovation in the emerging countries
New communication tools are all over. According to the providers there are more mobile phone contracts that living human beings on earth. Health services have not been spared by the association between medicine and communication tools. This combination is the bases of a new concept within the health services. This combination is within reach of emerging countries in so far that it could, even partially, reduce the sparsity of care and reduce the costs of the health systems and social security in HICs. This kind of medicine is only starting but the first results are promising. It seems without doubt that these forms of medicine will, in the long term, replace actual forms of medicine. Emerging countries have to adapt, secure and generalise these forms as to reduce the costs of the health system.
Preoperative application:
Several digital medical applications available on smartphone allow for an easier diagnostic and interpretation of the clinical exam in several specialties.
The haemodynamic parameters can be assessed by these applications. OpitBP allows for the measurement of the blood pressure and is comparable with a pressure meter (55). The Electro Cardiogram can be realised by watches connected to a smartphone (56). The same goes for some biological analysis like oxygen saturation and level of hemoglobin (57 -58). These innovations have a great impact on emerging countries where screening and routine exams are not accessible for the whole of the population (59).
Perioperative application
The availability of smartphone has the potential to revolutionize MIS by making it more accessible and feasible in emerging countries. Laparoscopy by smartphone has been described by Chatzipapas in 2017 (60). The system consists of a rigid laparoscope with a 0° lens of 10 mm diameter connected with, a made-on purpose, applicator to a smartphone. The light source is a rechargeable diode. Our department uses an old endoscopic eyepiece. This system allows for the replacement of the visual part of the endoscopic trolley (endoscopic camera, camera and unit, the monitor and the light source). The system has been validated in several specialties such as urology, gynecology, ORL, digestive surgery. In gynecology it permits hysteroscopic and laparoscopic diagnostic and simple surgeries like salpingectomies, detorsion of adnexa, drainage of abscesses, permanent tubal sterilization. This system is an autonomic one dispensing of the costly endoscopy turrets (Fig 3 a-3b).
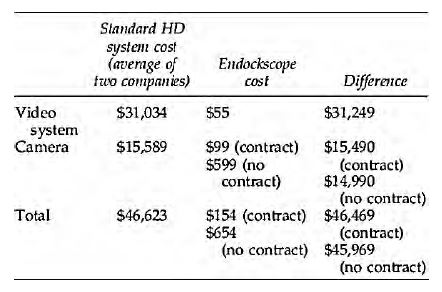
The cost of these turrets is around 50 to 70 times more expensive. (61). The smartphone will allow surgeons in the emerging countries to, in the future, have access to top technologies HD vision, 4K and even 3 D technologies. (62). The only limiting factor is the reduced live span of the mobile light source (Fig 4-5).
Postoperative application
These applications allow for observing the patients at distance after ambulatory surgery or even at home after being discharged. The registered information concerns: the temperature, the cardiac frequency, the oxygen saturation all of these are transmitted to the smartphone so that health care workers are rapidly informed in case of deterioration of the situation (63).
The smartphone can also be used as a tool to observe the importance of wound infection through image making and images captured and stored in the memory to compare in time or send to the medical and nursing staff. (64). This can be of pivotal importance is reducing the hospital stay but still maintaining adequate high-quality observation. Adapting these measures will in time allow significant reduction of the costs concerning surgical patients equally so in HICs as in LICs and LMICs countries (Fig 6).
Quality boost for initial and continuous education
The new numeric terminals can optimise the surgical training in the emerging countries and this using simulator made off materials that have been recycled and smartphones. The latter can replace at the same time the camera and the screen. The high-definition images can be transferred to larger screens (65 – 66). It has been proven that simulation boxes manually made out of recycled materials are as efficient as commercially available simulators (67) (Fig 7).
It would also be interesting to make instruments and objects for the simulation by 3D printing. The use of the miniaturized cameras allows for perfect mimic the use and the manipulation of the endoscopic camera in theatre (68). The introduction of “touch surgery” as a tool in the education process of future surgeons allows for a good involvement in the surgical universe and represents an interesting pedagogic instrument in the LICs and LMICs. (69). The world-wide connectivity through the existing technologies can also facilitate the teaching and the learning by developing tools with video capacity like FaceTime, Skype, Google Duo, Zoom and many others. These are able to allow for direct communication during consultation and guarantee a direct return of information. Tele learning and tele assistance would be appropriate in environments with limited resources. Labs for learning can be developed using databases and portable computers at low costs. (70 – 71 – 72 – 73).
Conclusion
Surgeons in LICs and LMICs have to adapt their equipment according to the local financial resources in respecting security.
Surgeons, decision makers and instrument makers have to work together more intensely with their focus on innovation to allow for access to surgery in the low-income countries and reduce the spending in the health services in the rich countries.
Key to success is the appropriate use of the local human and financial resources. In the future the surgeons will have to redefine the MIS as a surgery on measure of both the patient and the local circumstances and adapt MIS to reduced human and financial realities.
The learning institutions, medical faculties at universities and others in the LICs and LMICs will have to integrate courses focused on the economy of the health systems.
Acknowledgements:
The author wishes to thank Bruno J van Herendael for the translation of the article from French to English and Emmanuel Nzau Ngoma for his positive criticism and providing photographs.
References
Figure 1: The world map with the regions where people do have little or no access to surgery.
Figure: 2 G4 Indicating the surgical conditions and the number of deaths caused.
Figure 3 a: Simple solutions using a smartphone and adapter to the scope and a diode light source. (Photo courtesy Emmanuel Nzau Ngoma)
Figure 3 b: The screen of the smartphone is duplicated on the computer screen or any smart additional screen (Photo courtesy Emmanuel Nzau Ngoma)
Figure 4: The smartphone and the lightsource fitted on the hysteroscope with the obtained image seen on the laptop. (Photo courtesy Emmanuel Nzau Ngoma)
Figure 5: Clinical application of the simple system in theatre. (Photo courtesy Emmanuel Nzau Ngoma)
Figure 6: Indicating the difference in costs between the classical systems and the smartphone system.
Figure: 7 An example of a smartphone training set. The one in the figure is still quite sophisticated and can be made even simpler with recuperated less costly materials.