Authors / metadata
DOI: 10.36205/trocar1.2022001
Abstract
The #Enzian classification provides a complete assessment of superficial, deep and also extragenital endometriosis findings. In contrast to the rASRM classification, it is applicable both in the diagnostic setting (ultrasound and MRI) and intraoperatively.
Introduction
Endometriosis is the most common benign disease in gynecology.
The important symptoms are cyclic pain, bleeding disorder, infertility and organ destruction which can lead to an enormous reduction of the patients’ quality of life, sometimes even lifelong. The manifestations are very diverse. It primarily affects the organs of the internal genital tract, the peritoneum but also the neighboring organs in the small pelvis as well as extraperitoneal structures extending to the pelvic wall.
Endometriosis can also occur outside the pelvis (diaphragm, appendix, umbilicus, inguinal region, sacral nerves, lungs or abdominal wall etc.). The symptoms of endometriosis are influenced by the activity of the foci as well as, essentially, by the localization and size of the findings. Sometimes small peritoneal foci remain asymptomatic, whereas large ovarian endometriomas may cause complex symptoms (pain, sterility, hormonal imbalances, etc.).
Extragenital foci in the intestinal or bladder wall or even in the ureter result in functional problems of the affected organs. In the case of an involvement of the pelvic wall including the ureter, for example, there is a risk of chronic urinary retention with consecutive damage to the kidney, which is sometimes recognized much too late.
Adenomyosis, a special form of endometriosis in the uterine wall, is usually responsible for severe dysmenorrhea, bleeding disorders (hypermenorrhea) and subfertility. However, not all findings are symptomatic.
Therapy: In the absence of a clear theory of development, there is also no causal therapy to date.
Symptomatic endometriosis is treated either conservatively or surgically. Hormonal modulation or inactivation of proliferating endometriosis cells is sufficient in many cases.
This keeps the endometriosis inactive for the duration of the therapy, but does not destroy or even eliminate it. In contrast, elimination is achieved with surgical treatment of the disease, either by destruction or resection.
These procedures carry the risk that not all foci are/can be identified and removed intraoperatively, or that further problems may occur postoperatively due to complications. The recurrence rate after surgical interventions depends on the complexity of the disease but also on the most complete pre- and intraoperative identification of the foci and their complete removal. In any case, the most comprehensive preoperative (and intraoperative) diagnosis possible is essential.
Diagnosis
Correct diagnosis begins with a differentiated history and gynecologic examination and often ends with diagnostic laparoscopy. To this day, the latter is still considered the gold standard for diagnosing endometriosis, especially since it also involves tissue sampling with histological evidence of endometriosis.
The additional visualization of adhesions and the examination of the tubo ovarian unit (entity?) is very important, especially in infertile patients.
The fact that endometriosis is not only an intraperitoneal disease often leads to an incomplete detection of the disease during diagnostic laparoscopy.
Diagnosis has to include difficult-to-detect but symptomatic findings in the bowel wall and/or findings in the extraperitoneal space. The persistence of the disease and thus unsatisfactory surgical results are also due to inadequate diagnosis.
This eminent problem has been considerably reduced by improving the techniques of operative laparoscopy on the one hand and by very differentiated ultrasound diagnostics on the other. In addition, MRI examinations are very valuable in cases of unclear symptoms or specific clinical findings, especially for the visualization of extragenital foci.
Classification
For decades, attempts have been made to classify endometriosis by means of various classification systems in order to be able to make statements about the severity of the disease, the forms of therapy, the success, the recurrence rate after therapies and finally about the prognosis of the disease. Since 1979, the AFS/rASRM classification has been primarily used in the context of surgical intervention (laparoscopy, laparotomy) (1). However, among other classifications, especially the Enzian classification for deep endometriosis (DE) and the EFI (Endometriosis Fertility Index) for the assessment of chances to conceive in the presence of peritoneal/ovarian endometriosis are regularly used in clinical and scientific routine. This has also been recommended by various scientific societies.
As a further development of the Enzian classification, the #Enzian classification is now presented.
Strengths and weaknesses of these classifications
1)AFS/rASRM classification
The application of the AFS/ rASRM classification requires a surgical procedure to classify the intra-abdominal extent of the disease with involvement of the peritoneum, ovaries and fallopian tubes, as well as the adhesions. The lack of correlation of the rASRM stages with symptoms can be partly explained by the different pathophysiological behavior of the disease itself, but also by the incomplete documentation of the overall findings.
Thus, the clinical relevance of this classification or its value in the analysis of clinical and scientific studies, especially in cases of DE, must be critically questioned.
Grading based on rASRM level into only 4 stages (1-4) is far too inaccurate. The complex distribution system of the points to be assigned often leads to the fact that the staging is determined by estimation rather than by an exact calculation.
In a study with endometriosis specialists, the use of the three different classifications systems (rASRM, Enzian, EFI) was tested by means of the commonly used paper survey forms or by means of a computerized data collection program (EQUSUM). None(!) of the 40 endometriosis specialists succeeded in correctly classifying the clearly defined, fictitious cases using rASRM in paper form. Using the Enzian classification proved much easier and more accurate (2).
Problems with r ASRM in staging:
1.it is inappropriate for the detection of deependometriosis (DE).
2.there is a low correlation between stage andsymptoms
3.it cannot be used in diagnostic procedures(USD, MRI)
4.it does not allow prediction of prognosis
5.it is complex and difficult to use (especially, inpaper form)
2)The Enzian Classification (3, 4)
The Enzian classification was the result of an expert meeting held by the Endometriosis Research Foundation (SEF) in 2002 (1st Weissensee Meeting). This new classification assesses deep endometriosis in its totality and does not divide the disease into an overall stage. It was used in combination with the rASRM classification – to provide the most comprehensive description of the disease.
The substantial technical improvements in operative laparoscopy over the past 20 years allow for complete classification of deep endometriosis, although this may require invasive surgery. However, deep endometriosis can also be accurately visualized by non-invasive methods such as sonography and MRI diagnostics. These procedures also allow the use of the Enzian classification.
The Enzian classification is based on a topographic categorization (division?) of the pelvis into different compartments. In addition to the compartments designated with capital letters, all other extragenital lesions found are also documented according to location and size by means of the “code”. Only affected compartments are listed in the coding. The need to classify endometriosis in a such a differentiated manner has been investigated in several studies(5) (6) (7).
It has been shown:
1.certain affected compartments and thenumber of affected compartments correlate withsymptoms.
2.there are usually significant similaritiesbetween the anatomical (surgical) findings andthe findings obtained by sonography or MRI.
3.this classification allows an improvement ofinterdisciplinary therapy concepts.
4.the duration of surgery and the surgicaldifficulty correlate with the localization and theextent of the findings (Enzian) of the differentcompartments.
5.the risk for postoperative complications incomplex findings can be estimated. with theEnzian classification.
3)EFI ( Endometriosis Fertility Index) (8).
The EFI (Endometriosis Fertility Index) was developed in order to make a prognostic statement about the probability of pregnancy in endometriosis and infertility.
This multifactorial statistical model takes into account not only endometriosis but also other factors that limit fertility, such as the age of the patient, previous pregnancies, the duration of infertility, the state of the tubo-ovarian entity and finally the rASRM stage.
The points calculated in this process allow to give an estimation of the prognosis for a spontaneous pregnancy. However, of the maximum 10 points to be scored, only 2 points are given specifically for endometriosis staging. Thus, the EFI cannot be considered primarily as a specific endometriosis classification.
4)Recommendations
Recommendations from various societies point out the above problems and advocate the simultaneous use of multiple classifications or a single comprehensive classification (9, 10) (11). Surgeons, ultra-sonographers and radiologists succeed in visualizing and documenting the full extent of endometriosis. A common “language”, or classification, would be very useful (12).
5) The #Enzian classification
The original Enzian classification (without consideration of ovarian and peritoneal endometriosis and adhesions) was revised by a group of experts from SEF (Endometriosis Research Foundation) and by other international specialists and evolved into the #Enzian classification(13).
The new classification takes into account the different localizations and sizes of the lesions, including those that can be visualized in ultrasound(u) and MRI(m) examinations.
The individual anatomical regions are defined by capital letters and the size of the foci are divided into categories (1-3).
The classification aims to represent the entire extent of the disease in detail and not to reduce it to only e.g., 4 stages, which would cause a great loss of information.
The use of a code serves to present the entire findings in a more reproducible way.
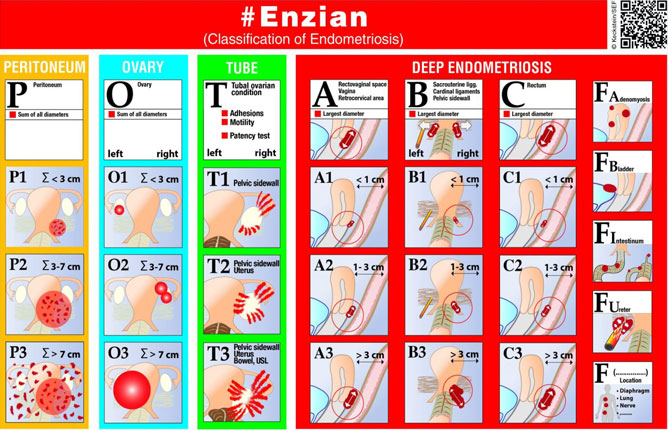
Figure 1: #Enzian classification. The different anatomical structures (compartments marked with capital letters) are systematically ordered next to each other. The size of the lesion, (1-3) is arranged from top to bottom. Special anatomical structures such as uterus, ureter, higher bowel segments, etc.) are additionally listed on the right.
These extragenital forms of the disease are labeled with the letters F such as FU= ureteral involvement with stenosis, FB = bladder endometriosis, etc….
6) Coding of the recorded findings:
P=Peritoneum (diameter of that circle in which the areas of all visible foci can be summarized fictitiously =Σ). P1=<3cm, P2=3-7cm, P3=>7,
Detection by surgery
O= ovary (sums of diameters of all endometriosis cysts; each side assessed separately; left/right)
O1=<3cm, O2=3-7cm O3=>7,
Detection by US/ MRI/surgery
T= adhesions and tubo-ovarian findings (adhesions of adnexa to pelvic wall, uterus and bowel, tubal patency= +/-; each side assessed separately; li/re).
T1= adhesions of ovary to pelvic wall
T2= adhesions of ovary, pelvic wall and uterus
T3= adhesions of ovary, pelvic wall, uterus and intestine
Detection by US/surgery
A/B/C = deep endometriosis
A= Retrocervical area, septum rectovaginale, vagina, B= parametrium, ligamentum sacrouterinum, C= rectosigmoid). Assessment of size, i.e., diameter as marked in Figure 2 in each case. Detection by TVS/ MRI/ surgery
F: FA= adenomyosis, FI= other intestinal lesions > 16 cm from anus, FU= ureter(left/right), obstruction, F(…)= defined other localizations.
Detection by TVS/ MRI/ surgery,
Options for classification/coding: surgical(s), sonographic(u) or by MRI(m).
#Enzian classification can be applied intraoperatively or by sonography or with MRI, and is annotated with the small letters: (s)= Surgery, (u)= Ultrasound, (m)= MRI
Each of these diagnostic methods has specific strengths and weaknesses. For example, peritoneal lesions cannot be visualized and classified sonographically, or occasionally a bowel lesion cannot be visualized and classified sufficiently well by diagnostic laparoscopy alone. A combination of the findings of the different methods is possible and also useful.
If anatomic structures cannot be assessed (e.g., due to extensive adhesions), the affected compartment is coded with an (x).
Only those compartments showing pathology are coded to make the extent of the disease with the affected organs easier and faster to understand when reading.
#Enzian (u), “Sonographic” classification:
Sonography can be used to visualize the ovaries (O), compartments A, B and C, uterus (FA), bladder (FB) and ureters (FU). Adhesions between the ovary, the pelvic wall, the uterus and the bowel can be described using dynamic ultrasonography, with the “sliding effect” as defined by the expert group IDEA (International Deep Endometriosis Analysis)
Good correlation between sonographic Enzian classification (old classification) and surgically obtained findings was demonstrated by Hudelist and al. (14).
In a retrospective study, the accuracy of the sonographic #Enzian classification(new classification) compared with that of surgery was demonstrated by Di Giovanni et al (15). Very similar significant results were shown in the prospective multicenter study by Montanari et al. using 745 patients from 7 centers with a proven expertise in the field of sonography and surgery (16) . This was confirmed by the study of Bindra et al. (17) recently.
These results support the ISGE recommendation for the documentation of endometriosis, which is based on the clearly structured systematics of the IDEA group and the #Enzian classification(18) (19). This especially underlines the importance of systematic recording and interdisciplinary communication.
The correlation between the Enzian classification of DE and the severity of preoperative pain symptoms have been shown by Haas and Montanari (20, 21) (22).
Operating times and risk of surgical complications can be predicted by the Enzian classification. Intra-operative Enzian classification as well Enzian findings in MRI correlated with the duration of the surgical procedure (20, 21). Poupon et al (23) used the Enzian classification to create a nomogram based on three criteria: the patient’s age, previous surgeries for DE, and the extent of disease described by the surgical Enzian classification. This provides the possibility to predict a surgical risk.
Imboden also used Enzian classification to analyze the risk of bladder dysfunction after surgery for deep endometriosis(24). (Author in the last paragraph are you talking on #Enzian or Enzian please clarify)
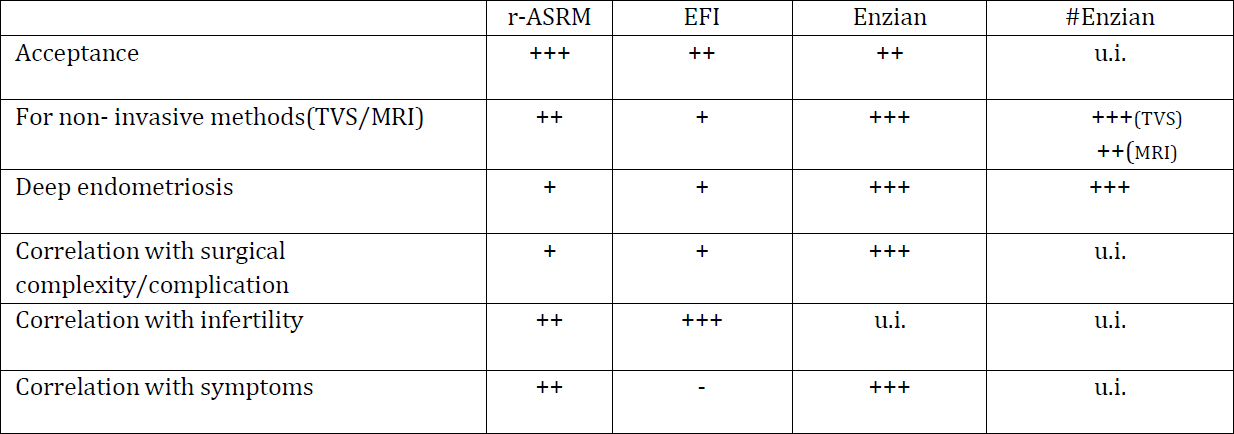
The #Enzian classification also includes peritoneal and ovarian endometriosis, adhesions in the adnexa and tubal patency. So far, there are no data on the ability of this classification to predict fertility. A comparison of the different classification systems (table1), rASRM, EFI and Enzian und #Enzian have was summarized by Hudelist et al. (6).
7) Application and examples:
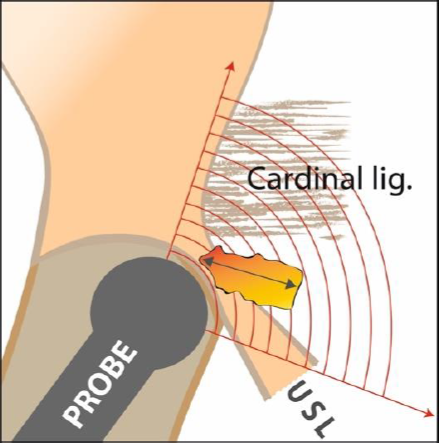
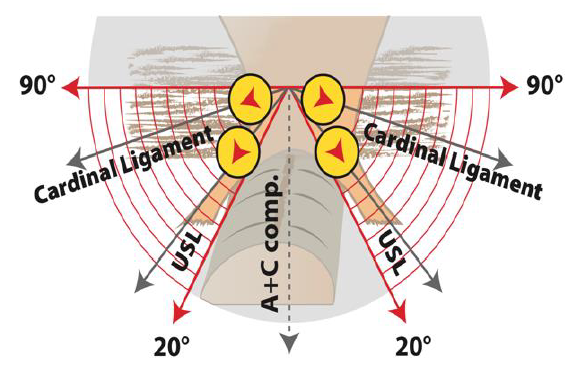
The possible application of the ultrasound probe in transvaginal ultrasound diagnostics is shown in Fig. 2 and 3.
#Enzian(m), MRI classification.
The accuracy of the diagnosis of endometriosis and systematic documentation with #Enzian (25) or Enzian has been demonstrated by several research groups (26) (27-30). The advantage of MRI examination is likely to reside in the assessment of uterine muscles, pelvic wall including nerves and extra pelvic findings such as diaphragm, lungs etc.
#Enzian(s), Surgical Classification:
Diagnostic/surgical laparoscopy has been the gold standard to definitively diagnose and classify endometriosis. To measure lesion sizes, the surgical instruments used (diameter 5 or 10 mm) serve as a reference measure, or a special measuring instrument is inserted into the abdomen. Visualization and evaluation of extraperitoneal structures, parametria to the pelvic wall, or intramural intestinal lesions (DE) cannot be fully appreciated by pure diagnostic laparoscopy. Accurate classification then requires a more invasive procedure with exposure of the structures and excision of the lesions if necessary. However, if a complete dissection is not necessary, not desired, or not possible, the unclear compartments within the #Enzian classification can be coded with an x (= not presentable) or the inclusion of sonographic(u) or MRI(m) findings can be made. This leads to a comprehensive view, allowing for interdisciplinary communication. The new #Enzian classification serves as a common language for diagnostics and therapy.
Summary
The #Enzian classification is the first comprehensive system to describe endometriosis as completely as possible and to provide a useful tool for various diagnostic procedures. The coding takes into account all affected anatomical structures, including the very complex manifestation of TIE and also less frequently detected localizations.
The possibility to use the classification also in the context of non-invasive diagnostics (ultrasound and MRI) and in combination with surgery simplifies the interdisciplinary procedure. A reduction of the collected findings to an overall stage (stage 1-4) as in rASRM is deliberately avoided in #Enzian in order to depict the extent of the disease in an optimal way.
The positive findings to date in the application of the #Enzian classification show good applicability and high accuracy with regard to the reproducibility of the findings and the correlation with the complexity of the disease and its treatment.
References
Figure 1 shows the schematic representation of the #Enzian classification and thus “coding formula”. (Fig1.)
Table 1: Advantages and disadvantages of the different systems (- not suitable, + little, ++ moderately and +++ well suited, among others, u.i. under investigation (6)
Figure 2: Sonographic measurement of the B compartment. Positioning of the ultrasound probe in the fornix, with a slight tilt and lateral positioning of the probe. The maximum length of the lesions is measured and coded with #Enzian (13).
The #Enzian coding in sonographic assessment is explained in figure 3. Figure 3: Illustration of the correct position of the probe during sonographic assessment of the USL and parametria= B compartment. In the range between 20 and 90° lateral to the sagittal plane, the entire B compartment is included. In the middle (sagittal section), the A and C compartments are assessed.
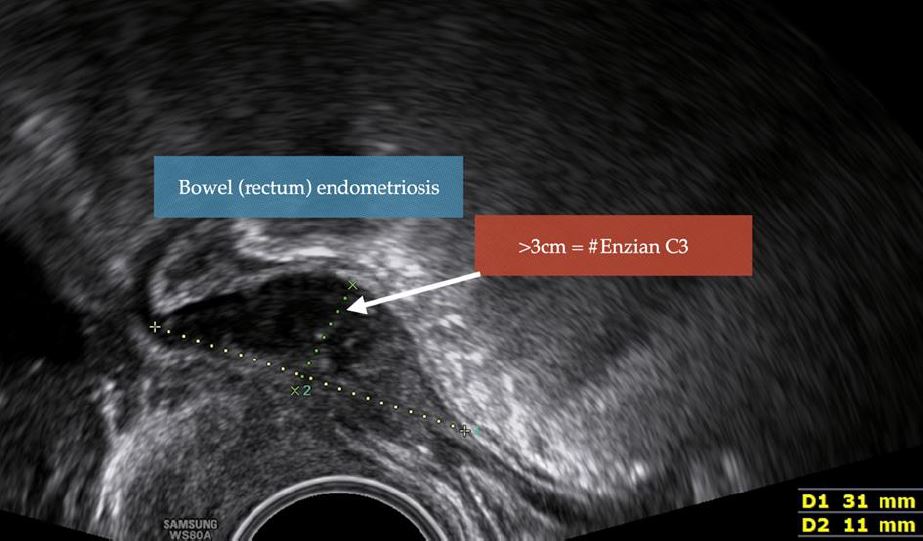
Figure 4: Example 1; Sonographic imaging and coding of DE of the anterior wall of the rectum, in sagittal section. The rectal wall is infiltrated by endometriosis (hypodense area represents the infiltration of the muscular layer) over a length of 3.1cm. Coding: #Enzian(u) C3.
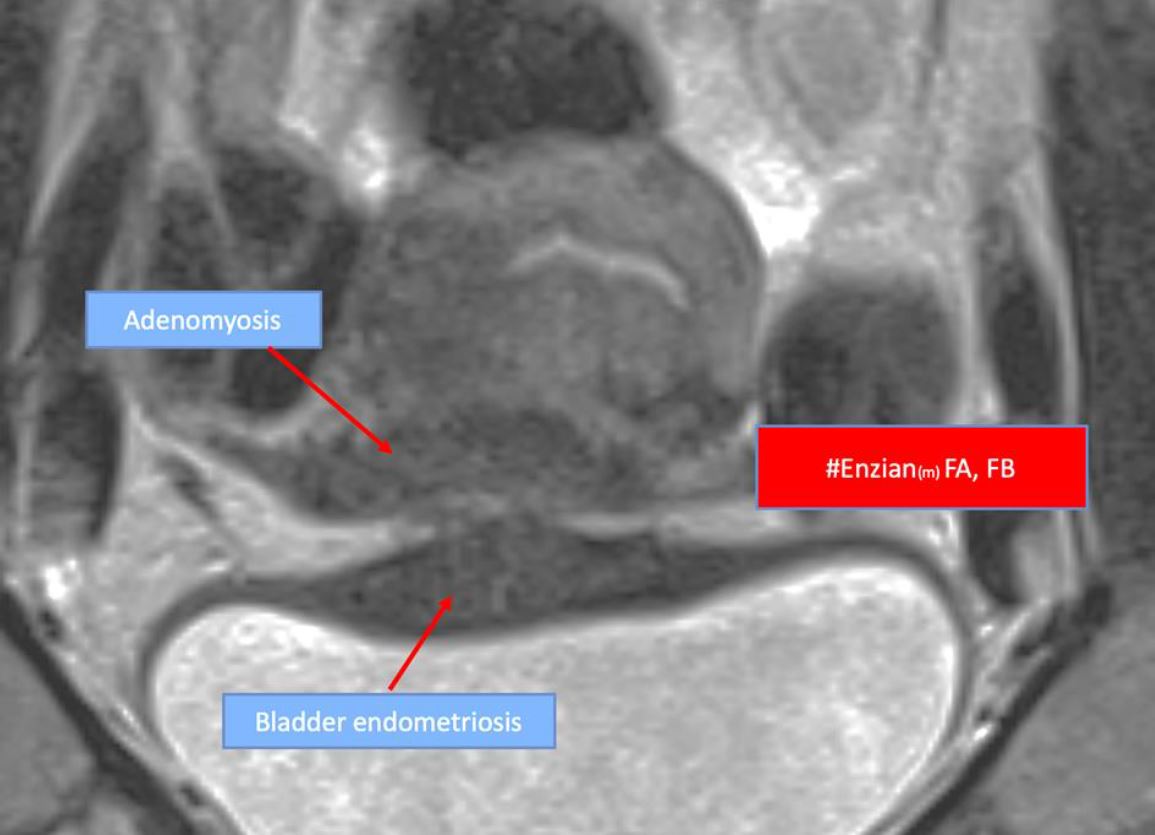
Figure 5: Example 2; MRI image showing adenomyosis and bladder wall endometriosis. FA: Adenomyosis, FB: Bladder endometriosis; Coding: #Enzian(m) FA, FB (Author I did put more contrast in the picture see if this is OKE for you)
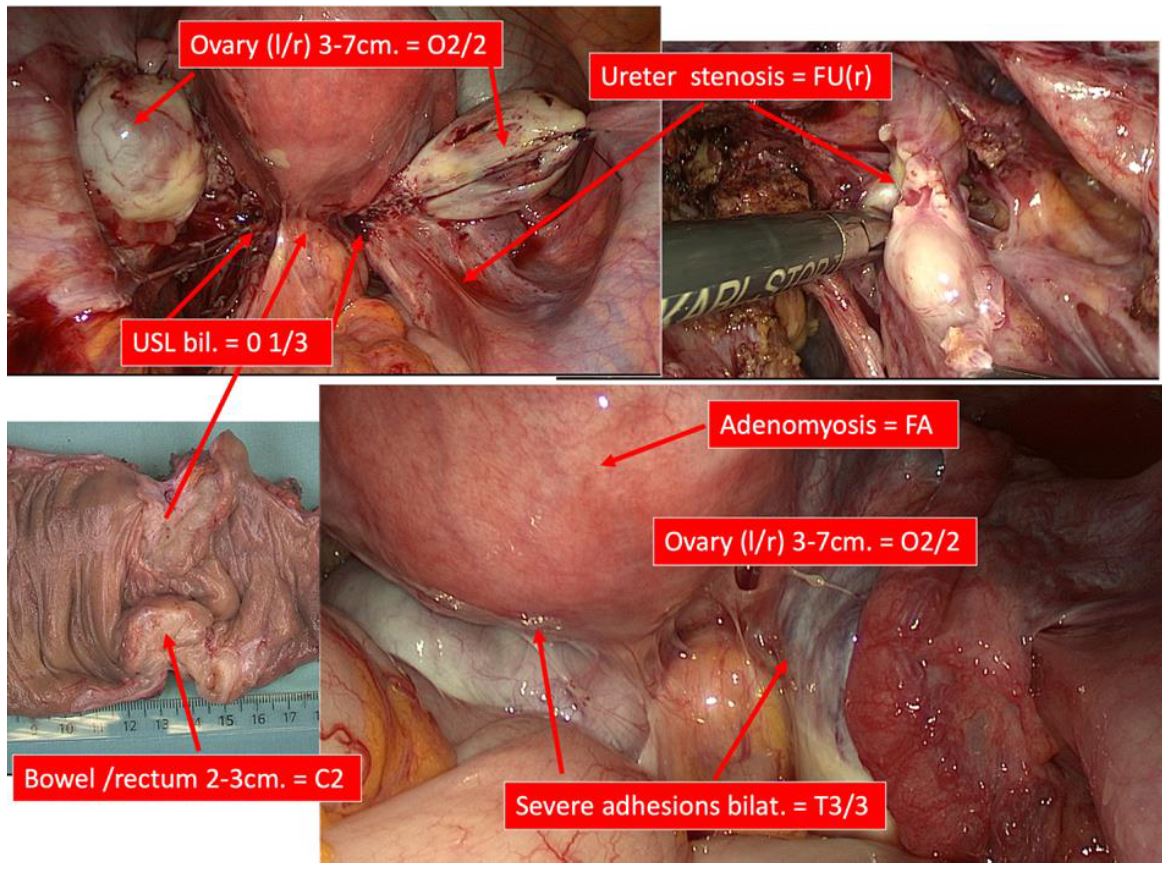
Figure 6: Endoscopic view with coding of the affected structures according to the #Enzian classification
P= Peritoneum: All foci shown have a combined diameter of 3-4cm = P2.
0= Ovary: endometrioma, diameter left 5cm, right 4cm = O2/2
B= USL: nodules in the liagamentum sacrouterinum (USL) left side > 1cm/ right side of 3,5 cm = B1/3
C= rectum: nodule of 2-3 cm = C2
T= Adhesions: between right and left ovary, uterus and pelvic wall and bwel = T3/3
FA= Uterus: adenomyosis (sonographically detected) = FA(u)
U= Ureter: intrinsic endometriosis right Ureter= FU(r)
Coding: #Enzian(s) P2, O2/2, T3/3, B1/3, C2, FA(u), FU(r).