Authors / metadata
DOI: 10.36205/trocar1.2021005
Abstract
The laparoscopic treatment of prolapse is dominated by Sacral colpopexy, the latter is known as current Gold Standard”. Various new approaches have been described in the last years with different fixation areas and different combinations. The ischial ligament is used successfully via vaginal route since a long time. We have developed a laparoscopic approach to use the structure for apical repair without mesh. This paper describes the technique and the first single center data for this new surgical technique.
Corresponding author: Sanjay Shanbhag e-mail: superstryker7@gmail.com
Introduction
As mesh Issues caused by vaginal approaches occurred in the last two decades, more laparoscopic procedures were developed and published[1-3].Most of them were mesh based using long mesh arms (Dubuisson) or the pectineal ligament (Noé). There is a long tradition for abdominal fixation (laparotomy and vaginal fixation either [4, 5]. The ischial ligament is successfully used uni- or bi-lateral since decades but has not been approached abdominally yet. Due to mesh discussion, we have adopted the thread based vaginal technique to an abdominal approach. According to Delancy there is evidence that the apex of the vagina (level 1 by delaneys classification) is at the level of S2 vertebra or at the level of ischial spine. Also, the mid portion of the vagina (level 2 Delaney) derives a lot of support from the white line over the obturator fascia. Both the ischial spine and the white line are anatomically bellow the obturator nerve. With the advent of high-definition cameras, these areas can be precisely dissected and thereby we have a concept of repairing the prolapse to correct the anatomical position. Since the braided polyester suture stimulates a reasonable amount of fibrosis, we use it to replace the lack of collagenization at the vaginal end.
Surgical approach and technique
Trocar position
1) A 10 mm optic trocar is placed in the midline one inch above the umbilicus.
2) One 5 mm trocar is placed above and lateral to the left anterior superior iliac spine for the surgeon’s left hand.
3) A second 5 mm trocar is added 2 inches to the left and two cm above the optical 10 mm trocar for the surgeon’s right hand.
4) A third 5mm trocar is placed just above the MacBurneys point on the right side for the assistant.
5) A Fourth 5mm trocar is placed two inches below and to the right of the umbilicus. This is exclusively used for the safe and comfortable passage of the 40 mm 1/2 circle taper cut heavy needle, attached to the number 2 braided polyester suture.
STEP 1: Dissection to approach the ischial bone
A 10 mm 50-degree scope is passed through a supraumbilical canula. The retroperitoneum is entered by cutting the round ligament on the right side and incising the peritoneum cranially parallel to the right infundibulopelvic ligament ( right ovarian vessels) and caudally to meet the uterovesical fold.
The para rectal space (Latzko’s space) is developed between the uterine and internal iliac artery (lateral border) and ureter (medial border).
Further dissection is carried out at a level caudal to the obturator nerve just lateral to the internal iliac artery and the umbilical artery.
The dissection is to be carried out with great caution taking very small steps and sometimes even excising small bits of the fat (in view of the vast variations in the anatomy as mentioned above), until the ischial bone is reached.
Further careful dissection of this part of the ischial bone anteriorly and parallel to the obturator nerve is commenced.
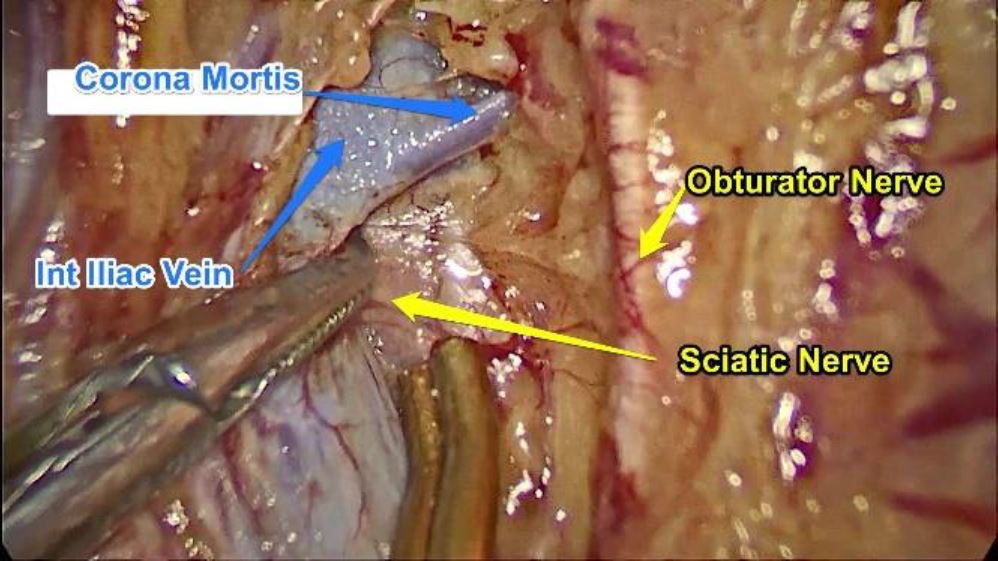
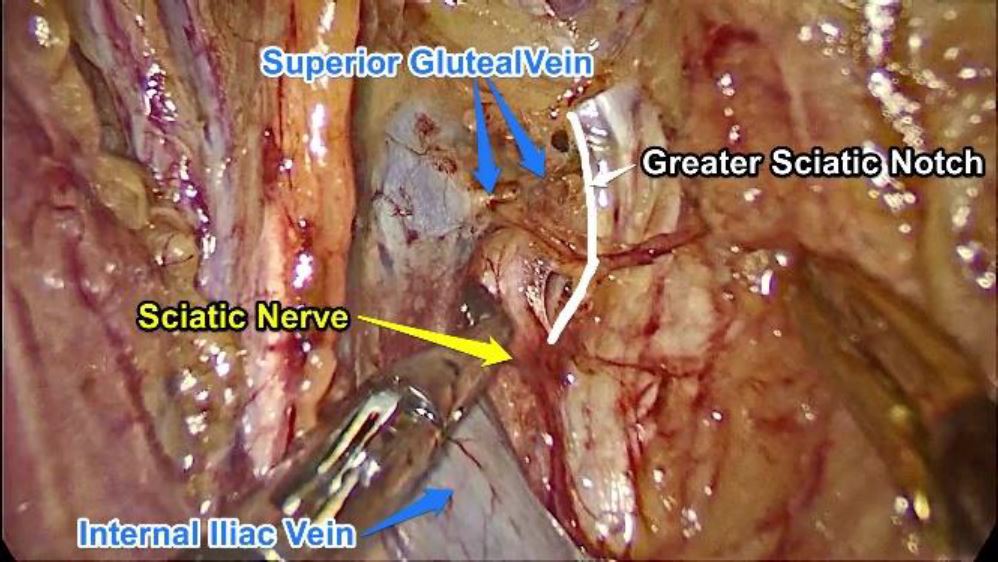
One may come across small branches of the obturator artery and vein or even the corona mortis which may have to be cauterized and cut to prevent soiling of the area. At this level the concerned strip of the ischial bone with its periosteal thickening is bordered by Obturator muscle anteriorly, the lumbosacral trunk, internal iliac vein and internal iliac artery posteriorly and the obturator nerve cranially as well as the greater sciatic notch caudally.
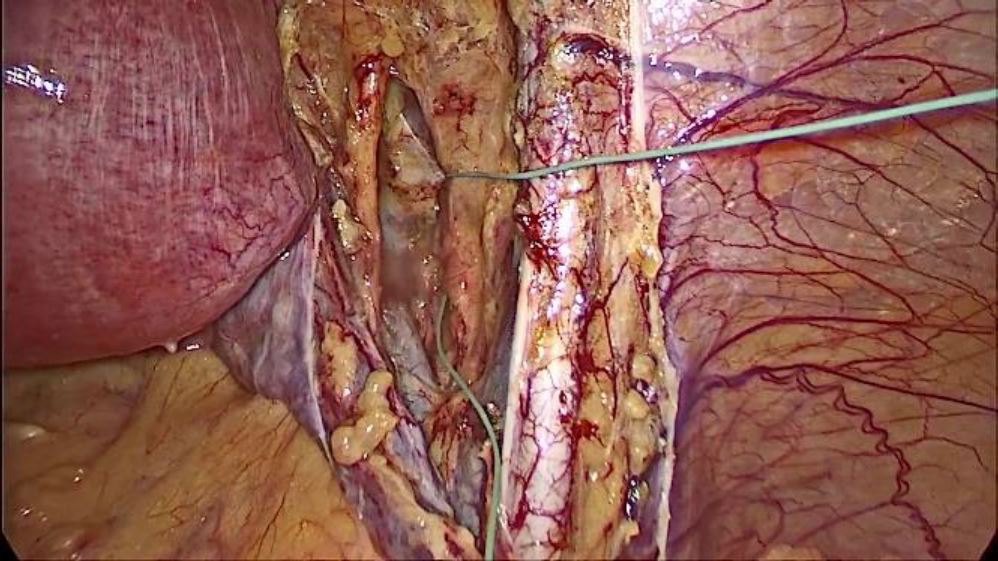
Fig. 1: Dissection area to approach the ischial spine
STEP2
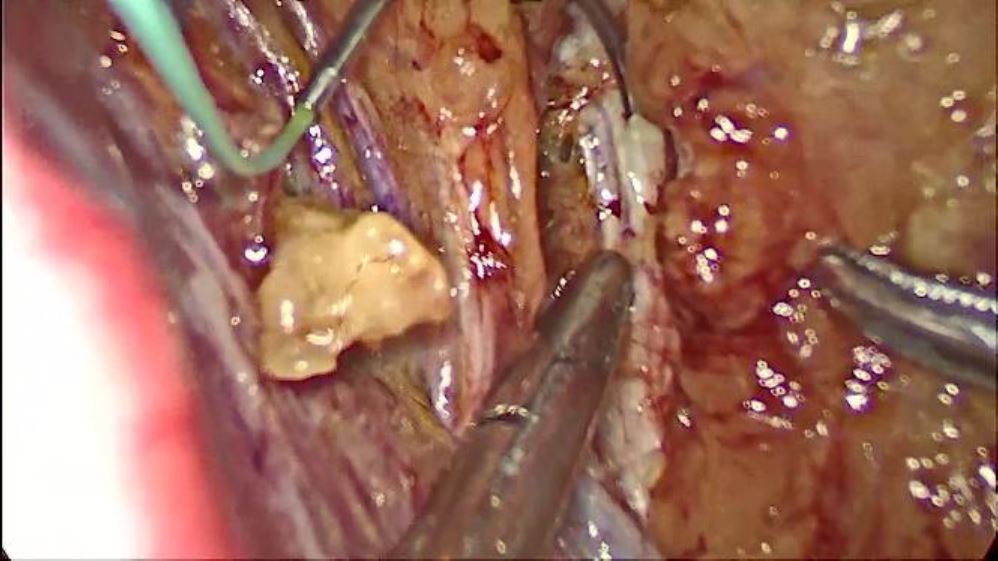
A 40 mm 1/2 circle taper cut heavy needle attached to the number 2 braided polyester suture of 75 cm length is taken.
The needle is passed directly through the anterior abdominal wall above the right anterior superior iliac spine, thus ensuring that only the requisite suture material is intra-abdominal to prevent it from entangling and facilitating handling of the long single strand which will be used for further surgery.
The needle is then passed through the thickened portion of the periosteum above the ischial bone previously exposed using a laparoscopic needle holder passed through the fourth 5mm port described above.
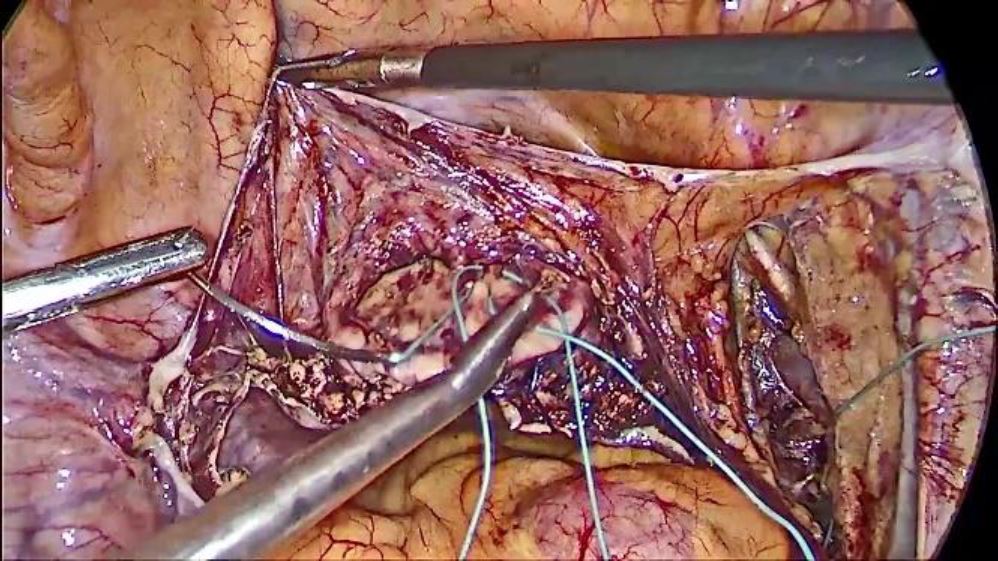
Fig. 2: Needle and thread placement
STEP 3
The 10 mm 50-degree scope is replaced with a 10mm 30-degree scope. A total hysterectomy is achieved if the patient is perimenopausal as it facilitates the further surgery. The vaginal vault is sutured in two layers to reduce the extrusion of the poly-filament polyester suture.
STEP4
A 1.5-inch broad malleable copper retractor is introduced into the vagina from bellow. This facilitates the further dissection and suturing.
The vesico vaginal space is dissected out up to the trigone of the bladder. The peritoneum on the posterior vaginal wall is cut above the fat and the rectovaginal space is dissected out up to the lowermost part of the prolapse (not up to the levator ani) as guided by the assistant’s finger behind the malleable retractor.
STEP5
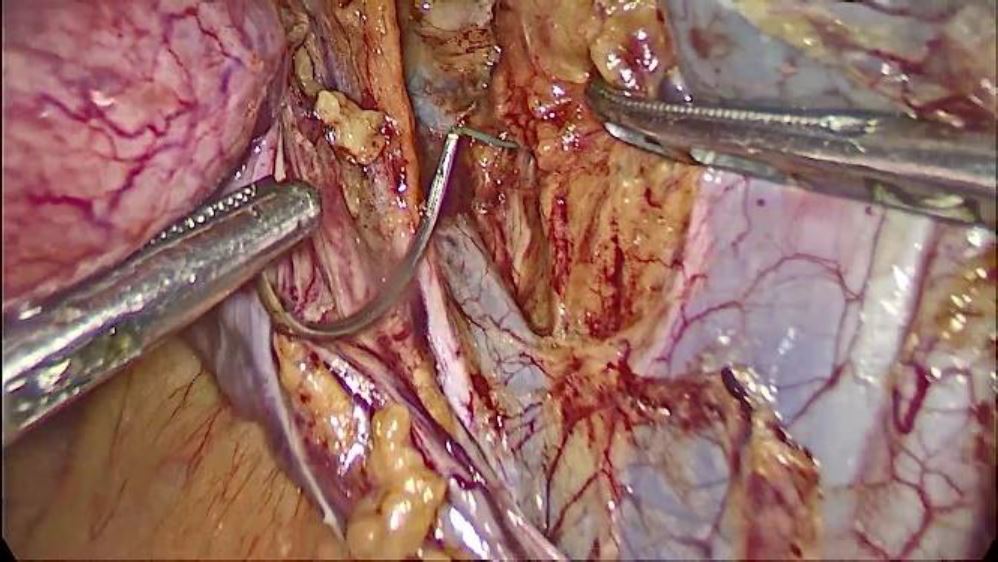
The aforementioned needle on polyester which is already passed through the thickened periosteum of the ischial bone is now passed by multiple bites through the fascia on the anterior vaginal wall (plication of fascia) taking care not to enter the vagina avoiding full thickness bites.
The suture material is deliberately kept on the right side of the operative field to avoid entangling. Bites are taken in a parallel manner to facilitate laparoscopic suturing. The polyester suture is pulled through to leave at least about 30 to 35 cm to do a similar plication of the posterior vaginal wall fascia.
The suture on the anterior vaginal wall is now pulled to tighten the plicated area thus correcting the cystocoele. The needle is now held and passed in a manner similar to the anterior vaginal wall, posteriorly starting from fascia over the lowermost part of the prolapsed posterior vaginal wall (as guided by the assistant’s finger placed posteriorly behind the malleable retractor).
Sequential bites are taken at multiple points in the fascia over the posterior vaginal wall (taking care not to entangle the suture) thus plicating the posterior vaginal wall and tightened effectively correcting the rectocele and enterocoele.
Special care must be taken at the area of the posterior fornix not to take full thickness bites as that part of the vagina is likely to be the thinnest.
A single bite is now taken in the anterior vaginal wall fascia (So that the subsequent knot lies anterior to the vaginal vault suture line and the suspension bridge from the ischial bone remains well above the right ureter) and 3 to 4 knots are tied to the afferent suture coming from the ischial bone so that even if the polyester suture is extruded, the suspension from the ischial bone remains in place.
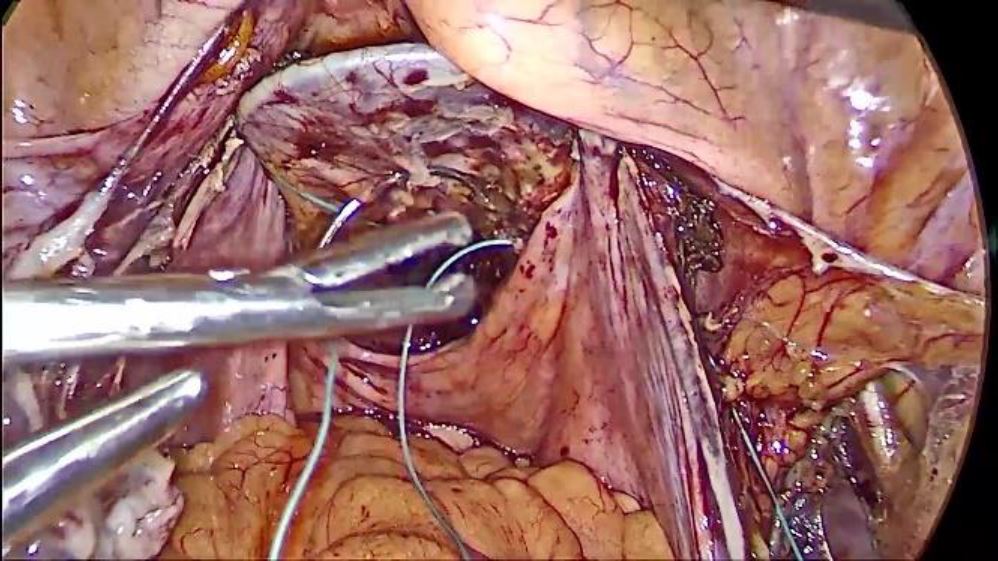
Fig. 3 Attachment to the vault after vaginal dissection
STEP 6
Now the suture is tied securely to the end coming into the abdomen (The suture end passing into the ischial bone) thus binging the vaginal apex to the S2 level. The excess suture from both ends and the needle are cut and removed from the abdomen.
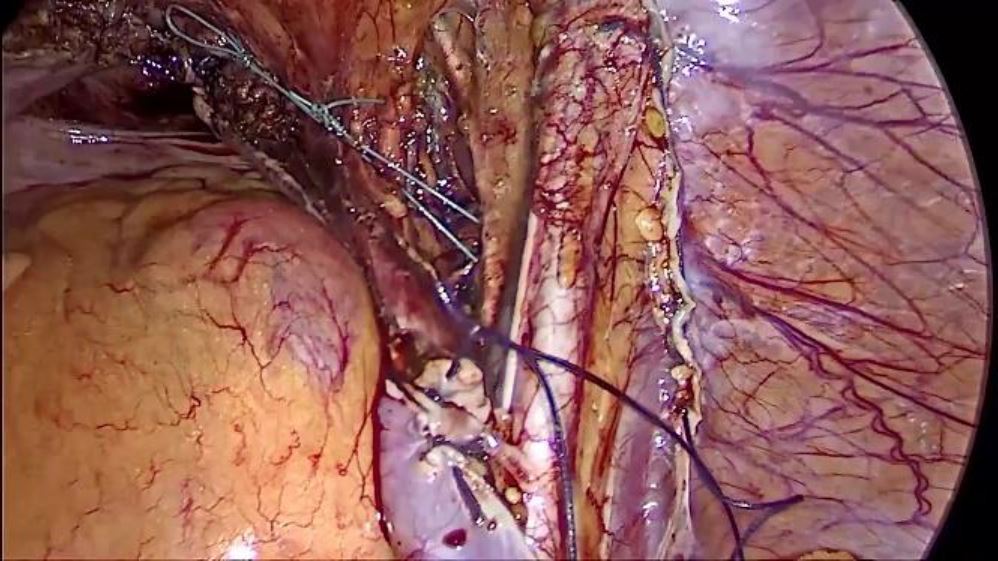
Fig. 5: Tightening of the thread to stabilize the apex
STEP 7
The entire peritoneum which has been opened from bellow the round ligament on the right side to the round ligament on left side is closed with 1-0 polyglycollic acid (Vicryl) in such a manner that the whole polyester suture and suspension system lies retroperitoneal.
This must be done meticulously as the polyester incites severe fibrosis and if exposed causes severe intestinal adhesions.
Fig.6: Closure of the peritoneum
Material and Method
We have followed up the patients one week, six months, one year and two years after surgery. The surgery was performed in 46 cases over a period of 3 years.
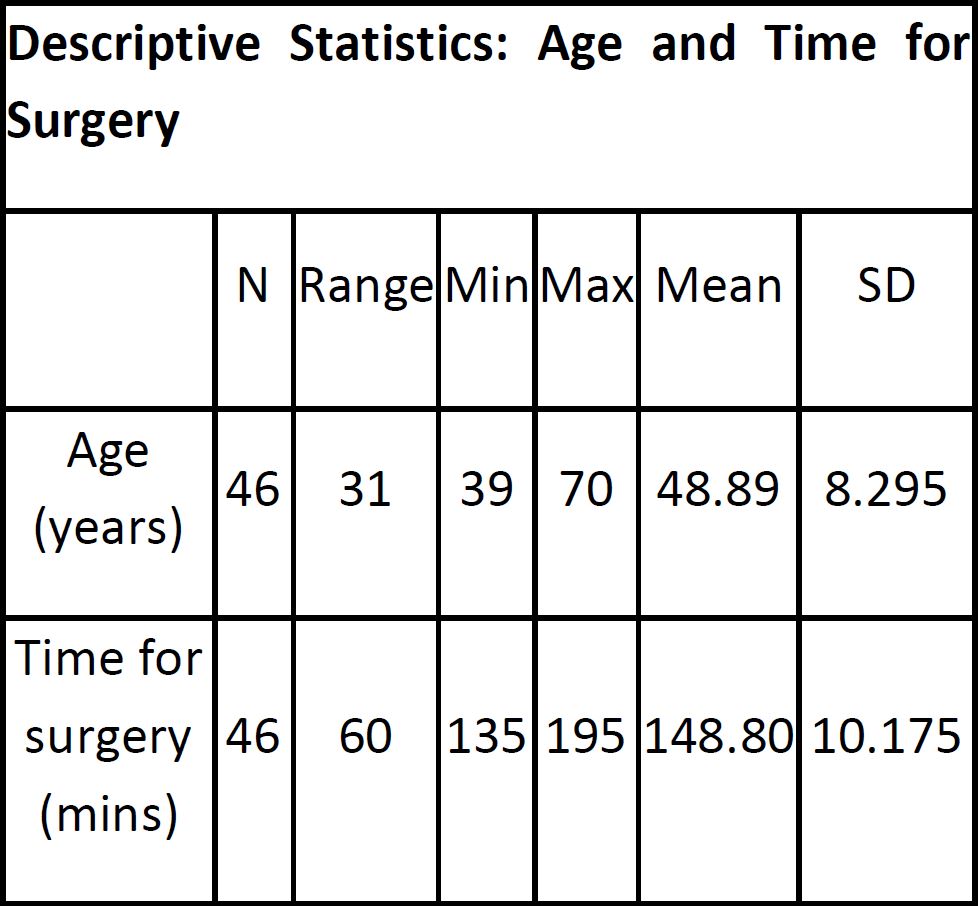
Table 1 shows the age of the patients and time taken for the surgery.
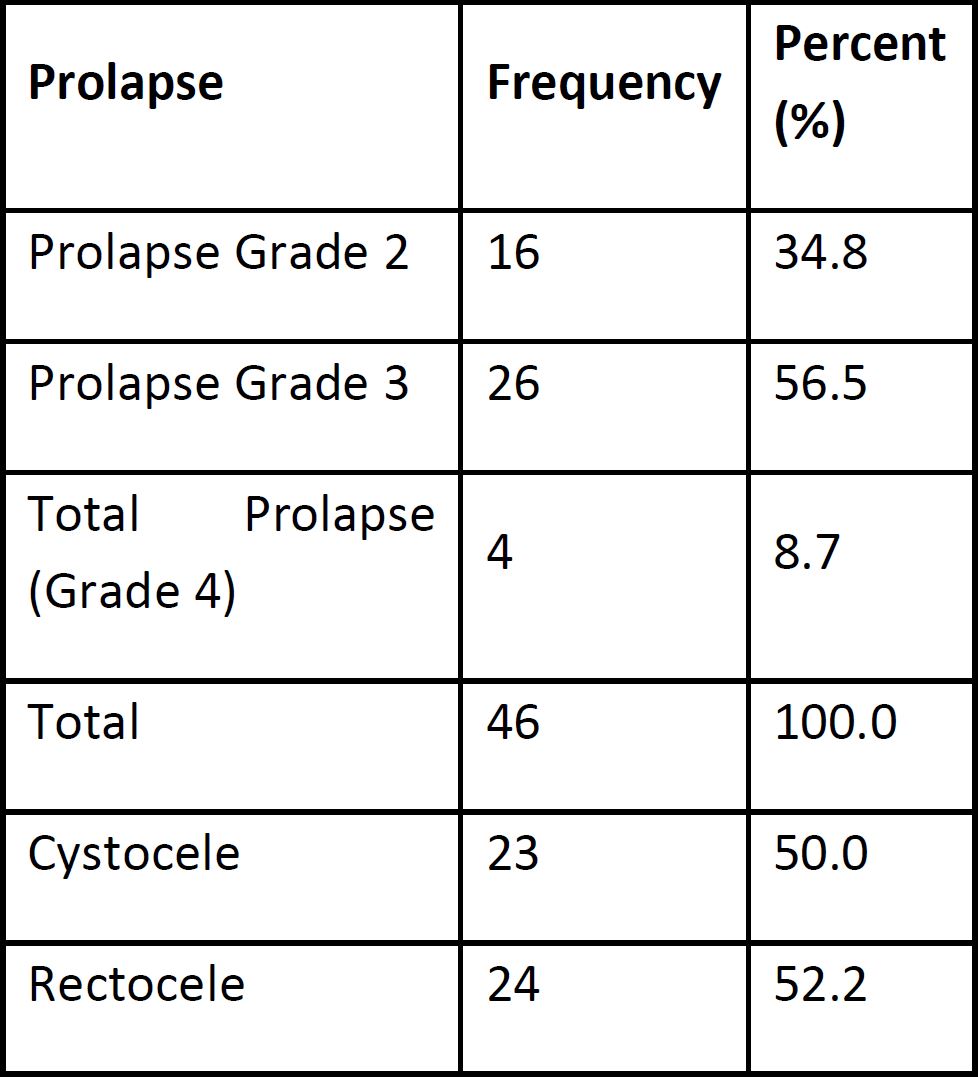
The distribution of the stages of prolapse and defects is listed in Table 2.
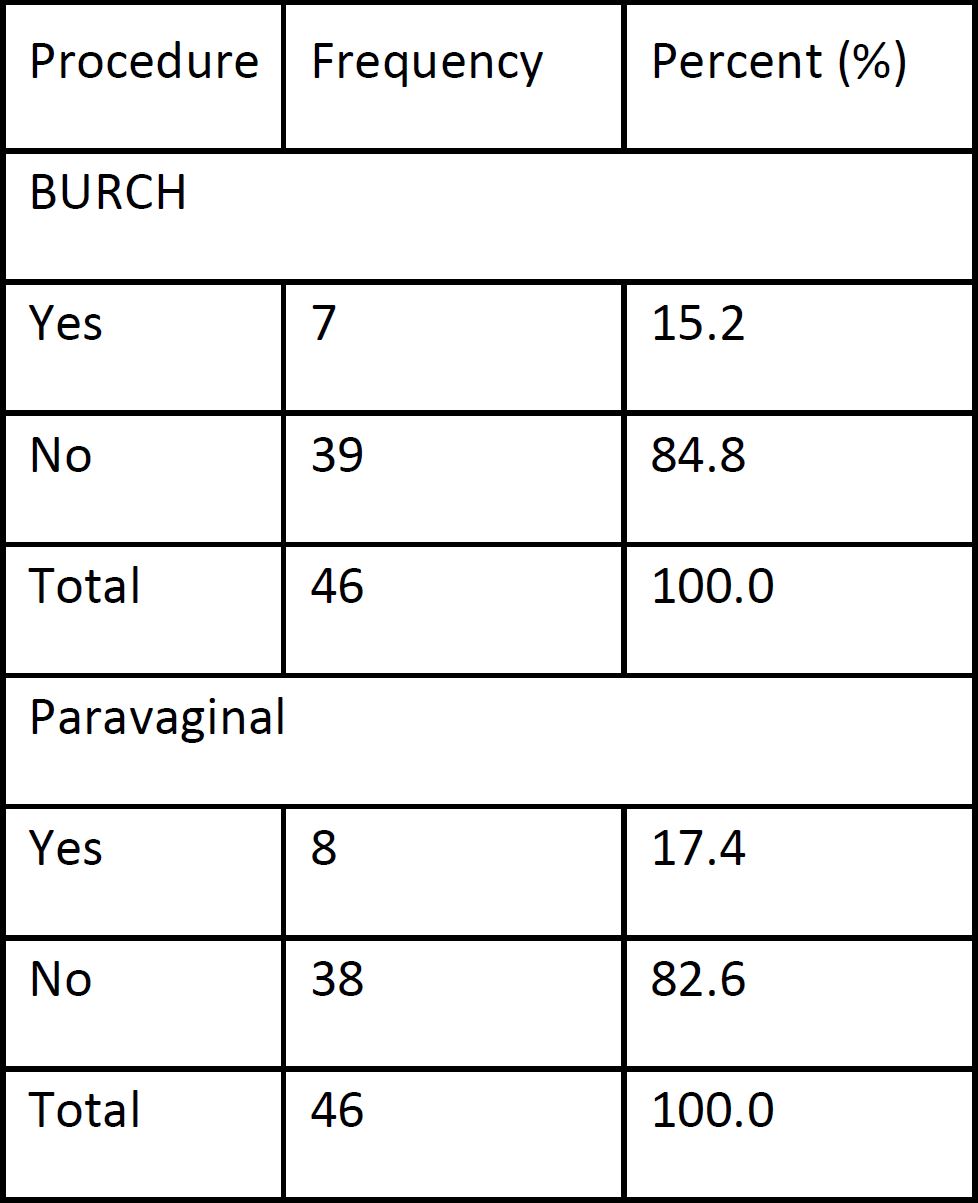
According to further symptoms we combined the ischial colpopexy with Burch colposuspension or lateral defect repair. The patients were assessed preoperatively for Stress urinary incontinence and those with genuine stress incontinence underwent Burch colposuspension. Those with lateral wall defects were further examined on table after the primary surgery (Ischial colpopexy). Suitable candidates further underwent a paravaginal repair.
Results
Complication: In 4.3% (2) of cases two major complications occurred (Obturator vein injury). These could be managed intra-operatively without any consequential damage. Smaller complications such as wound infections or urinary tract infections occurred very rarely.
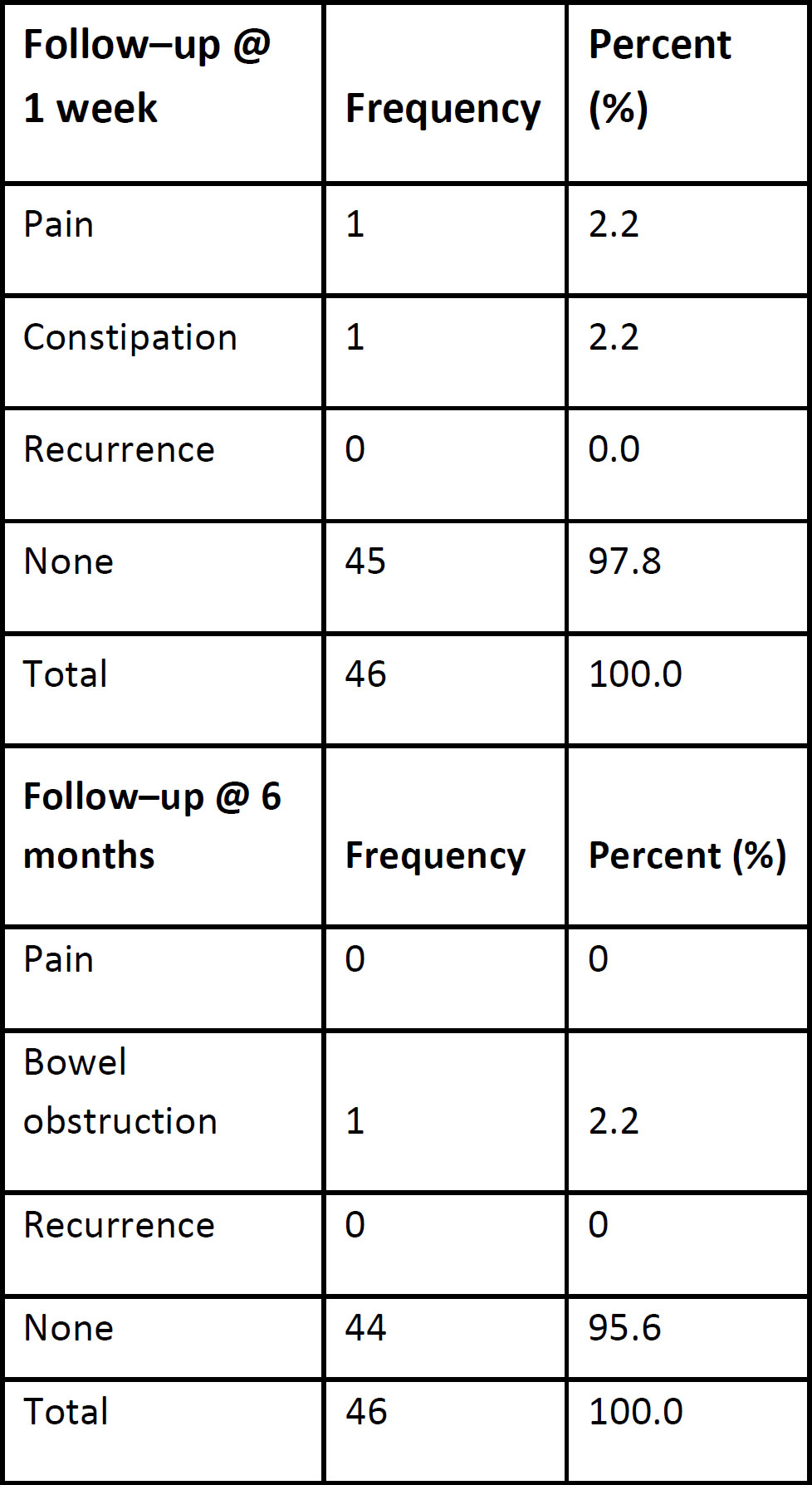
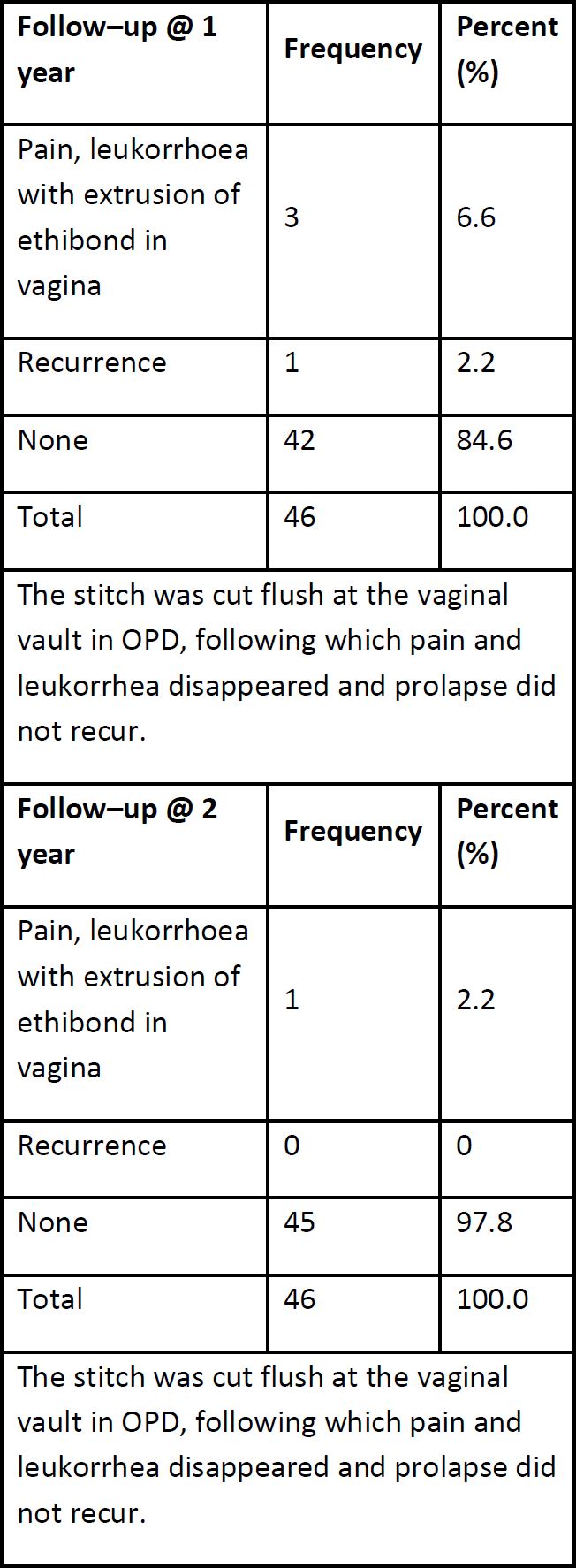
Follow-UP: In the first (one week) follow no recurrence was measured. One patient complained about pain and one about constipation (Table 4). After 6 months still no recurrence was seen but one major bowel obstruction. By reviewing the surgical video, we realized that the peritoneum was not sutured back properly. After one year 8.8% of the patients had an adverse outcome. One due to relapse and 3 due to exposure of the polyester thread with pain and leucorrhea. One year later no additional recurrence occurred but one more thread exposure, finally 8.8% after 2 years while the recurrence rate was only 2.2%.
The patient with bowel obstruction received a second laparoscopy 2 months after the first surgery where it was found that loops of ileum were adherent to the exposed polyester suture at the site of the knot. The patient with suture exposure were treated by excising the exposed thread without recurrence.
Discussion
Laparoscopic ischial colpopexy is a new approach for prolapse repair. The laparoscopic ischial colpopexy is a new approach to prolapse correction. The ligament has been used in vaginal surgery to fix the apex for decades. However, the laparoscopic approach has not yet been described. The technique was carried out early on and was described in the literature in 1981[6]. 2001 Lantzsch et al. Described urinary tract infection (n = 16, 8.0%), temporary irritation of the sciatic nerve (n = 15, 7.5%), temporary partial ureteral obstruction (n = 11, 5.5%) and less blood loss than 400 ml (n = 7) 3.5%) as operative complications (n = 200)[7]. In comparison, our operative complication rate is very low and must therefore compete with today’s procedures such as sacropexy, pectopexy and lateral suspension. Compared to the procedures mentioned, our complication rate remains low. This is of course the small number of cases and the implementation by a very trained surgeon is of limited significance[8-11]. Lantzsch et al. reported that 119 of 123 patients were completely healed with no evidence of urinary incontinence or prolapse. At the follow-up examination, 4 patients (3.25%) had a recurrent vaginal vault prolapse. Recurrent cystoceles, rectoceles, enteroceles were found in 10 cases (8.1%), (0.8%), (0.8%). The follow-up period in this study was 4.8 years on average. In comparison to the data from Lantzsch and the data from comparable laparoscopic studies, our success rate in the examined collective is very satisfactory. However, since we wanted to work without mesh, the high exposure rate of 8.8% must be viewed critically.
Limitations of the technique: The thread material is supposed to produce good fibrosis, but appears to favor exposure due to its strong local irritation. Therefore, we have to look for alternatives regarding the material. The suturing technique appears to be effective in correcting even a combined prolapse. However, the proximity to the ureter, pelvic floor nerves and lymphatic tissue requires a high level of expertise from the surgeon, which will make it more difficult to spread.
Conclusion
The laparoscopic ischial colpopexy can expand the portfolio of laparoscopic techniques for correcting pelvic floor defects. The early experiences with the technology show the feasibility but also the limitations. The material and safety of the technology still has to be examined on a larger scale before further statements can be made. Polyester sutures seem to be of risk to be used close to the vagina.